Generic Drugs: What They Are, How They Work, and What You Need to Know
When you pick up a prescription, you might see a generic drug, a medication that contains the same active ingredient as a brand-name drug but is sold under its chemical name. Also known as non-branded medication, it works the same way in your body—just at a fraction of the cost. The FDA requires these drugs to meet the same standards for safety, strength, and quality as the original, but many people still wonder: are they really the same?
Not all generic drug competition, the presence of multiple manufacturers producing the same drug leads to lower prices. Sometimes, when only one or two companies make a generic, costs stay high. That’s why some medications still cost hundreds of dollars even after the patent expires. And while most generics are safe and effective, generic medication errors, mistakes caused by confusing drug names or packaging happen more often than you think. Look-alike, sound-alike names like Hydralazine and Hydroxyzine have led to dangerous mix-ups in hospitals and pharmacies. These aren’t rare cases—they’re preventable, and they’re happening right now.
Another big concern is drug interaction, when one medication changes how another works in your body. A generic version of a statin might be fine on its own, but if you’re also taking an antifungal, the combo could cause muscle damage. The same goes for blood thinners and acid reducers. The active ingredient is identical, but the fillers, coatings, or release mechanisms can vary slightly—and those small differences matter. That’s why switching generics without talking to your doctor can be risky, especially with drugs that have a narrow therapeutic index, like warfarin or thyroid meds.
People often assume generic means cheap and low quality, but the real story is more about access and system design. generic drug savings, the billions saved annually by using non-brand medications help keep insurance premiums down and make treatment possible for millions. Medicare Extra Help, for example, cuts copays for generics to under $5 a pill for low-income seniors. But savings don’t mean you should accept any version without checking. Manufacturing flaws, like those flagged by the FDA in 2025, can affect purity or potency. Lot numbers matter. Recalls happen. And if you’re on multiple meds, tracking changes in how you feel after a switch can be the difference between a smooth transition and a hospital visit.
What you’ll find below isn’t just a list of articles—it’s a practical guide to navigating the real world of generics. From how to spot a dangerous interaction between your blood pressure pill and a new antifungal, to why your antidepressant might not work the same after a generic switch, to how market forces keep prices high even when dozens of companies make the same drug—this collection cuts through the noise. You’ll learn what to ask your pharmacist, how to read a recall notice, and why your symptom diary might be the most important tool you have when switching meds. No fluff. No marketing. Just what you need to stay safe and get the most out of your prescriptions.

How to Verify the FDA Orange Book for Generic Equivalence
Learn how to use the FDA Orange Book to verify if a generic drug is therapeutically equivalent to its brand-name counterpart. Understand TE codes, search steps, and common pitfalls to ensure safe substitutions.
Read More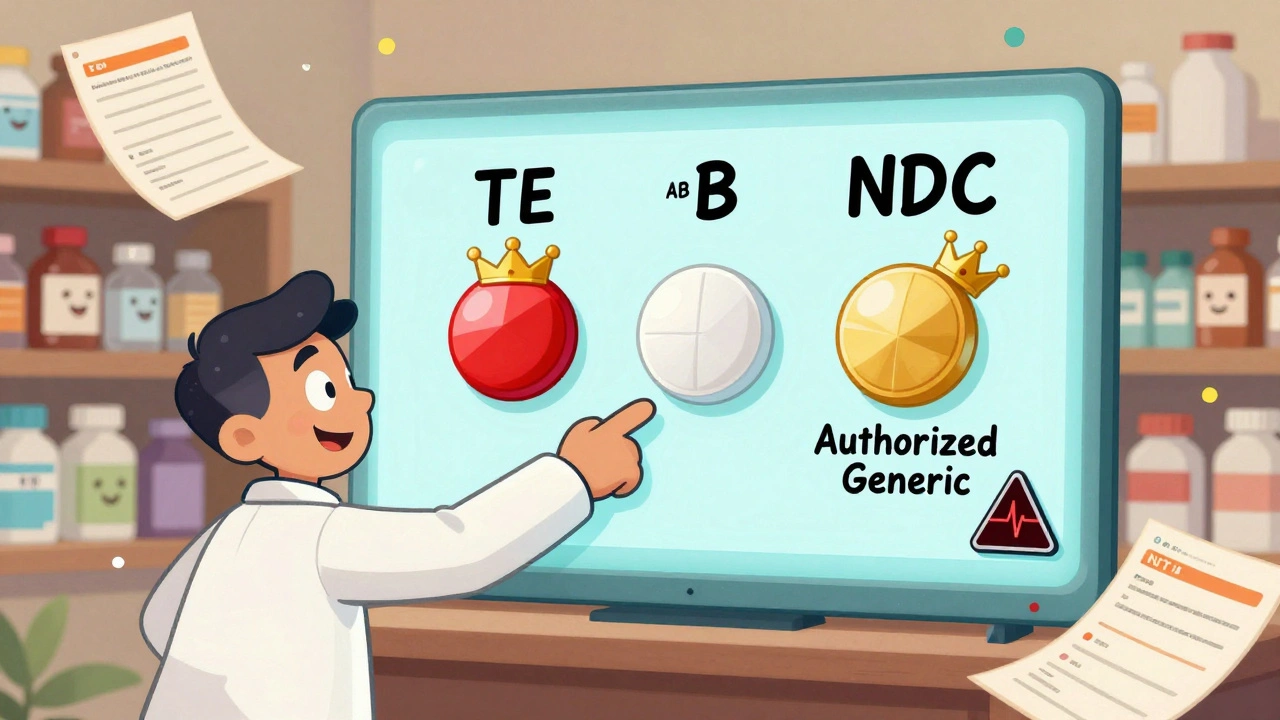
Generic vs Brand Identification in Pharmacy Systems: Best Practices for Accurate Medication Management
Learn how pharmacy systems accurately identify generic and brand-name drugs using NDC codes, TE ratings, and FDA guidelines. Best practices for safety, cost savings, and patient trust.
Read More
Pharmacy Margin Economics: How Generics Drive Profits in Today’s Drug Market
Generics make up 90% of prescriptions but drive 96% of pharmacy profits due to high markups on low-cost drugs. This article explains how PBM reimbursement, consolidation, and transparency shape pharmacy economics today.
Read More