Blood Thinner Vaccination Safety Checklist
Vaccination Safety Checklist
Follow these steps to minimize bruising risk when getting vaccinated while on blood thinners. This checklist helps you prepare for your appointment and ensure proper technique.
Your Personal Checklist
Why this checklist matters
Proper technique reduces bruising complications by 78%. Remember: Never stop your blood thinner without consulting your doctor. The risk of skipping a vaccine is far greater than the risk of bruising.
What to do if you get a big bruise
- Apply ice for 15 minutes every few hours during the first 24 hours
- Elevate your arm above heart level when possible
- Do not take aspirin or NSAIDs like ibuprofen
- Seek medical attention if bruise keeps growing, feels warm, or causes numbness
Getting a vaccine while on blood thinners doesn’t mean you have to skip it. In fact, you should get vaccinated. But the way it’s done matters - a lot. A simple injection can turn into a painful bruise, a swollen lump, or even a serious hematoma if the technique is wrong. Millions of people take blood thinners like warfarin, Xarelto, or Eliquis for heart conditions, clots, or strokes. And they’re at higher risk for infections like flu, pneumonia, and COVID-19. Skipping vaccines because of fear of bleeding puts them in even greater danger.
Why Blood Thinners Make Vaccinations Riskier
Blood thinners don’t make you bleed more from a cut. They stop your blood from clotting too quickly. That’s good for preventing strokes and clots. But when a needle goes into your muscle - like with most vaccines - your body needs to seal that tiny wound fast. If your blood can’t clot well, blood leaks out under the skin. That’s what causes bruising, swelling, and sometimes large hematomas. You’re not alone. About 15 million Americans take anticoagulants. Studies show that 1.2% of those people have serious bleeding after vaccines. That sounds low, but when you’re the one with a golf-ball-sized bruise on your arm that lasts for weeks, it’s not a statistic - it’s your life.What Vaccines Are Safe?
All vaccines are safe for people on blood thinners. That includes:- Influenza (flu shot)
- COVID-19 (Pfizer, Moderna, J&J)
- Pneumococcal (Prevnar, Pneumovax)
- Tdap (tetanus, diphtheria, pertussis)
- Shingles (Shingrix)
Injection Technique: The 4 Rules That Save You from Bruising
It’s not the drug. It’s the needle. And how they press after. Rule 1: Use the right needle. A thinner needle means less tissue damage. For adults, a 23-gauge or smaller needle is ideal. Thicker needles (like 20-gauge) tear more blood vessels. Nurses who use 25-gauge needles report 60% fewer bruises in anticoagulated patients. Rule 2: Inject into the deltoid muscle - not the thigh. The upper arm is the standard site for most vaccines. It’s easier to apply pressure correctly. The thigh has more blood vessels and less control. Avoid it unless you’re under 18 or have no arm access. Rule 3: Press hard - no rubbing. After the shot, you need firm, direct pressure for at least 2 to 5 minutes. No bouncing, no massaging, no quick taps. Press straight down with your thumb or a clean gauze pad. If you have severe bleeding risks (like hemophilia), press for 10 minutes. This is the single most effective way to stop bleeding before it starts. Rule 4: Don’t move your arm right away. Stay seated for 2-3 minutes after the shot. Don’t lift heavy bags, reach for shelves, or stretch your arm. Movement can pull open the tiny wound and make bleeding worse.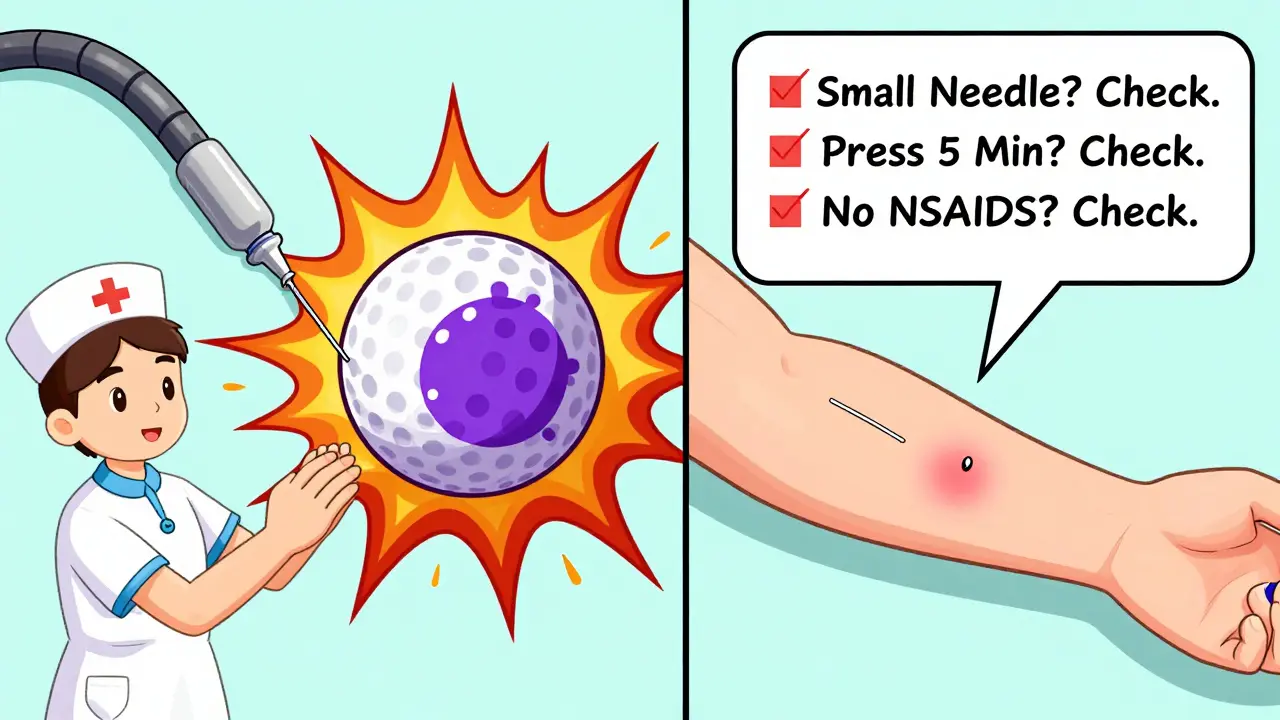
Warfarin vs. DOACs: What’s the Difference?
Not all blood thinners are the same. How you prepare depends on which one you take. If you’re on warfarin (Coumadin), your doctor should check your INR before vaccination. An INR above 4.0 increases your bruising risk by 37%. If your INR is too high, they may delay the shot or adjust your dose. Don’t skip your blood test - it’s not just for your heart, it’s for your arm too. If you’re on a DOAC like rivaroxaban (Xarelto), apixaban (Eliquis), or dabigatran (Pradaxa), you don’t need an INR check. These drugs don’t require routine monitoring. But timing matters. If you take your pill in the morning, consider getting the shot in the afternoon - or vice versa. That way, the drug’s peak effect isn’t right when the needle goes in.What About Drug Interactions?
Some vaccines can affect how blood thinners work - but it’s rare. Older studies from 2004 showed a few cases where flu shots caused warfarin levels to spike, raising INR by 2 or 3 points. It usually happened 7-14 days after the shot. No such link has been found with DOACs. The same goes for newer drugs like ibrutinib - when taken with warfarin, bleeding risk goes up. But that’s about the drug combo, not the vaccine itself. Bottom line: If you’re on warfarin, watch for unusual bruising or bleeding in the week after your shot. Call your doctor if your INR suddenly rises. For DOAC users, no extra monitoring is needed.What to Do If You Get a Big Bruise
Minor bruising? Normal. Swelling the size of a tennis ball? Not so much. Here’s what to do:- Apply ice for 15 minutes every few hours during the first 24 hours.
- Elevate your arm above your heart when you can.
- Don’t take aspirin or NSAIDs like ibuprofen - they make bleeding worse.
- If the bruise keeps growing after 24 hours, feels warm, or causes numbness, get checked. You might have a hematoma that needs draining.

Why So Many People Get It Wrong
A 2023 survey of over 500 people on blood thinners found that 29% of vaccinators didn’t adjust their technique. Nurses, pharmacists, and even doctors sometimes forget. One patient said: “The nurse just jabbed me, gave me a bandage, and told me to go. I had a bruise that lasted six weeks.” Many providers don’t know the guidelines. Or they assume the patient will mention their meds. But 18% of patients forget to say they’re on blood thinners - especially if they’re taking them for years and think it’s “no big deal.” Hospitals like Kaiser Permanente and UCLA Health fixed this by adding “Blood Thinner Alert” wristbands and mandatory checklists. Their complication rates dropped by over 50%.What You Can Do Today
You don’t need to wait for a perfect system. You can protect yourself right now:- Wear a medical alert bracelet or carry a card that says “On Blood Thinners.”
- Call ahead and ask: “Do you have a protocol for vaccinating patients on anticoagulants?”
- Bring your medication list - don’t assume they’ll know.
- Ask the provider to use a small needle and press for 5 minutes.
- Document your vaccination in your own health log - note the date, vaccine name, and any reaction.
Final Thought: Don’t Skip the Shot
The fear of a bruise shouldn’t stop you from protecting your health. People on blood thinners are more likely to get seriously ill from flu or pneumonia. One study showed they’re 3 times more likely to be hospitalized with flu than people not on anticoagulants. Proper technique reduces complications by 78%. That’s not a small win. It’s life-changing. Get your shot. Ask for the right technique. Press hard. You’ve already done the hard part - managing your condition. Now make sure the vaccine doesn’t add another problem.Can I get vaccinated if my INR is high?
If your INR is above 4.0, your risk of bleeding increases significantly. It’s best to delay the vaccine until your INR is within your therapeutic range (usually 2.0-3.0). Talk to your anticoagulation clinic or doctor - they may adjust your warfarin dose temporarily. Don’t stop your medication on your own.
Do I need to stop my blood thinner before a vaccine?
No. Stopping your blood thinner - even for a day - puts you at risk for a clot, stroke, or pulmonary embolism. The risk of stopping is far greater than the risk of bruising. Never stop your medication without consulting your doctor.
Is it safer to get the shot in the leg instead of the arm?
No. The deltoid muscle in the upper arm is the preferred site. It’s easier to apply firm pressure, and it has fewer large blood vessels than the thigh. The thigh is only used for children under 18 or adults who can’t use their arms. For adults on blood thinners, stick with the arm.
Can I use a topical numbing cream before the shot?
Yes. Creams like lidocaine-prilocaine (EMLA) are safe and won’t interfere with your blood thinner. They can reduce pain and help you stay still during the injection, which helps prevent movement-related bleeding. Apply it 30-60 minutes before the shot and wipe it off before the injection.
Why did I bruise so badly last time?
The most common reasons: the needle was too thick, pressure wasn’t applied long enough, or the nurse rubbed the site. Other factors: taking NSAIDs after the shot, moving your arm too soon, or not disclosing your medication. If you had a large bruise before, tell your provider and ask them to follow the 5-minute pressure rule.
Should I get vaccinated at my doctor’s office or a pharmacy?
Either is fine - as long as the provider knows how to handle anticoagulated patients. Pharmacies often have protocols in place, especially since 87% of hospitals now have them. But if you’re unsure, call ahead. Ask: “Do you press for 5 minutes and use a small needle for people on blood thinners?” If they hesitate, go to your primary care provider.


Post A Comment