Ulcer Management: Effective Treatments, Lifestyle Tips, and What Really Works
When you have an ulcer, a sore in the lining of your stomach or small intestine that causes burning pain, especially when your stomach is empty. Also known as peptic ulcer, it’s not just stress or spicy food—it’s often caused by H. pylori, a bacteria that weakens the protective mucus layer in your gut or long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen or aspirin, which irritate the stomach lining.
Ulcer management isn’t about waiting for the pain to go away. It’s about stopping the damage, killing the bacteria if it’s there, and giving your stomach time to heal. That usually means a combination of proton pump inhibitors, medications that shut down acid production so your lining can repair itself, antibiotics for H. pylori, and avoiding triggers like alcohol, smoking, and caffeine. Many people think antacids are the answer, but they only mask the problem. True healing requires targeting the root cause. If you’ve been told your ulcer is "just from stress," that’s outdated. Science shows H. pylori causes up to 90% of cases. And if you’re taking NSAIDs daily for arthritis or headaches, you’re at higher risk—even if you feel fine.
What you eat matters, but not in the way you might think. No, you don’t need to live on bland rice and boiled chicken forever. But skipping meals, eating late at night, or drinking coffee on an empty stomach can make things worse. The goal isn’t to restrict everything—it’s to reduce irritation while your treatment works. Some people find relief with probiotics or honey, but those are supports, not cures. The real fix is medical: getting tested for H. pylori, taking the right antibiotics at the right dose, and sticking with your PPIs long enough. Most ulcers heal in 6 to 8 weeks with proper care. Left untreated, they can bleed, perforate, or even lead to stomach cancer.
You’ll find real stories here—people who thought their pain was just indigestion, only to find out it was an ulcer. You’ll see what treatments actually worked, what didn’t, and why some meds like domperidone or propranolol show up in discussions even though they’re not direct ulcer treatments. Some posts dig into how other conditions like gastroparesis or diabetes affect healing. Others compare pain relievers and explain why some are safer than others. This isn’t a list of quick fixes. It’s a practical guide to understanding your ulcer, working with your doctor, and making smart choices so it doesn’t come back.
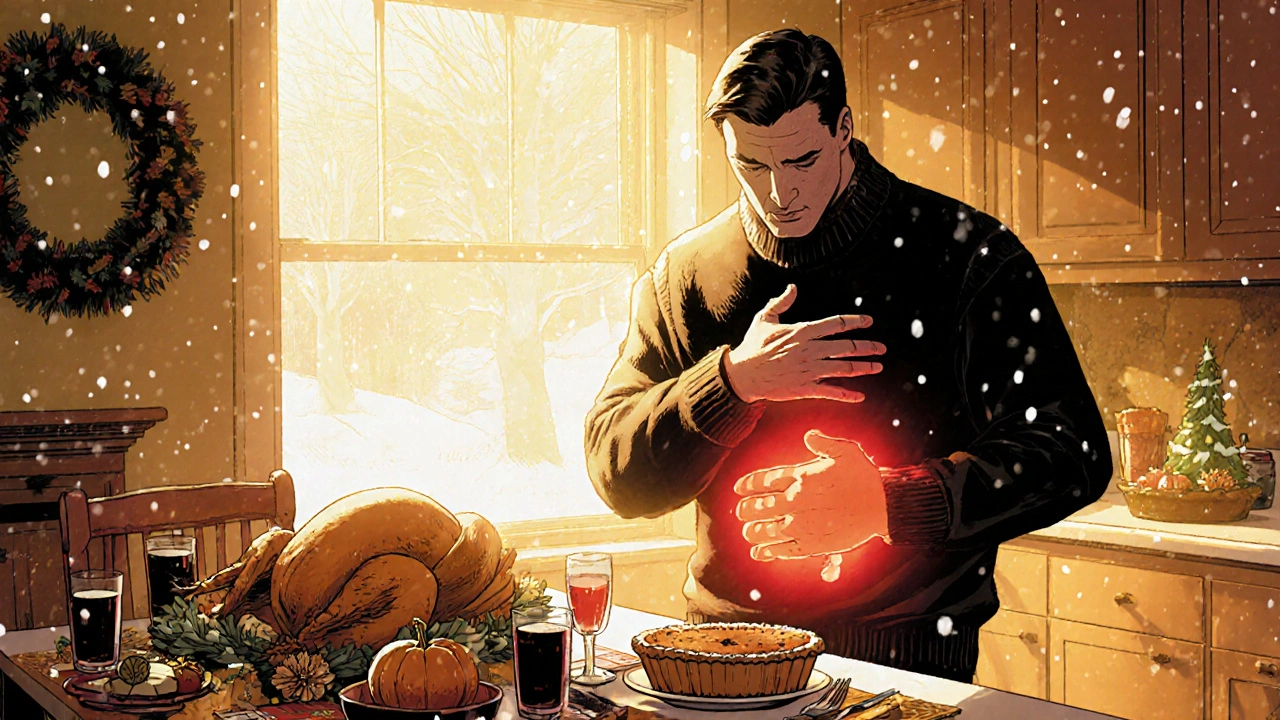
Holiday Ulcer Management: Keep Stomach Sores in Check
Learn practical steps to keep peptic ulcers under control during festive gatherings, covering diet, meds, stress, and red‑flag symptoms.
Read More