Personalized Dosing: Tailoring Medication to Your Body and Needs
When we talk about personalized dosing, the practice of adjusting medication amounts based on a person’s unique biology, weight, age, kidney function, or genetics. Also known as individualized dosing, it moves away from the one-size-fits-all approach that’s been common for decades. It’s not magic—it’s science. Think of it like setting the right temperature for your home: what works for your neighbor might leave you shivering or sweating. The same goes for drugs. A dose that’s perfect for one person could be too weak or dangerously strong for another.
DOAC dosing in obesity, a key example of personalized dosing in anticoagulant therapy, shows how weight and body composition change how drugs behave. For instance, apixaban and rivaroxaban work just fine at standard doses in obese patients, while dabigatran increases bleeding risk in severe obesity. No need to crank up the dose—just pick the right drug. Then there’s combination therapy, using lower doses of multiple drugs to reduce side effects while keeping effectiveness high. It’s used in high blood pressure, diabetes, and even depression. Instead of one big pill that knocks you out, you get two smaller ones that work together cleanly. This isn’t just theory—it’s what doctors are doing right now to keep people safer.
Personalized dosing isn’t just for complex cases. It’s also behind why some people get sick from a drug their friend took without issue. It’s why pharmacists check your kidney function before prescribing certain antibiotics. It’s why your doctor might ask about your diet, supplements, or even your sleep habits before writing a prescription. The goal isn’t to overcomplicate things—it’s to cut out guesswork. When you take the right amount of the right drug at the right time, you get better results and avoid hospital visits from avoidable side effects.
Below, you’ll find real-world examples of how personalized dosing plays out in practice—from how obesity changes blood thinner use, to why some psychiatric meds shouldn’t be swapped for generics without caution, to how tracking symptoms helps fine-tune treatment. These aren’t abstract ideas. They’re stories of people who got better because their meds were matched to them—not the other way around.
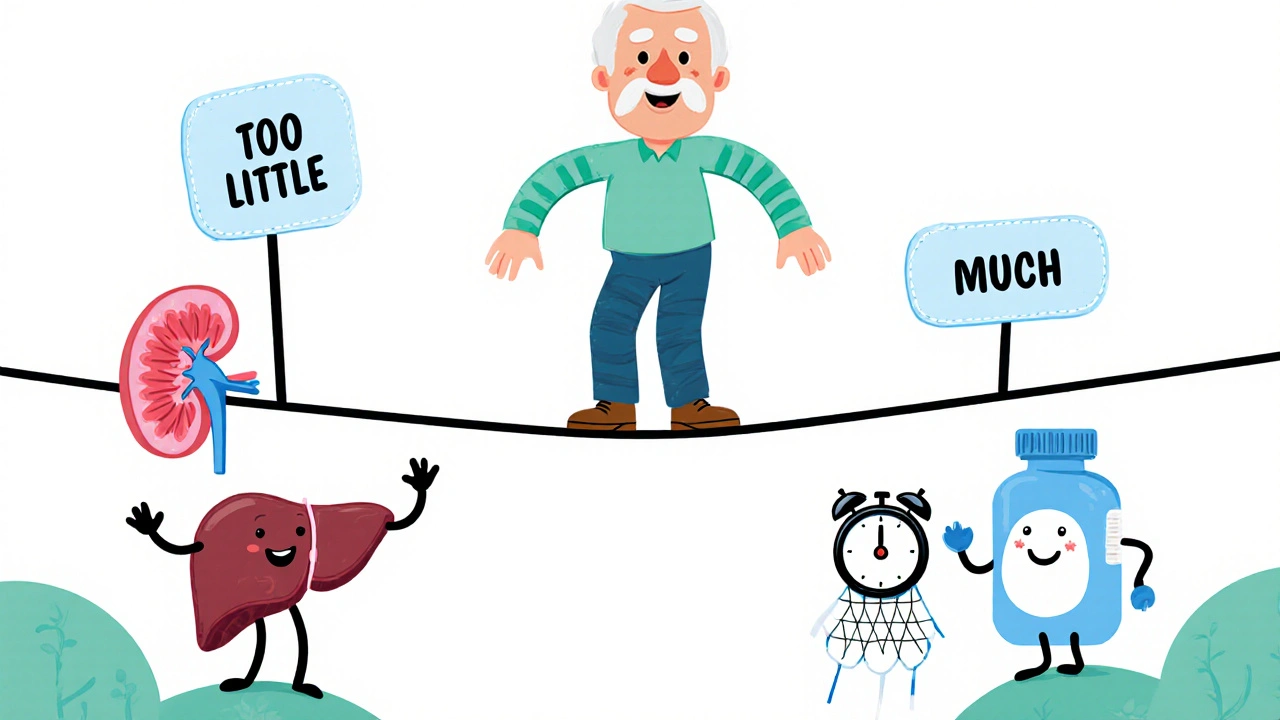
Adjusting Medication Dose: How to Find Your Safe and Effective Balance
Finding the right medication dose is critical for safety and effectiveness. Learn how age, kidney function, genetics, and drug interactions affect your dose-and what steps you can take to avoid dangerous side effects.
Read More