Narrow Therapeutic Index Drugs: What You Need to Know About Risky Medications
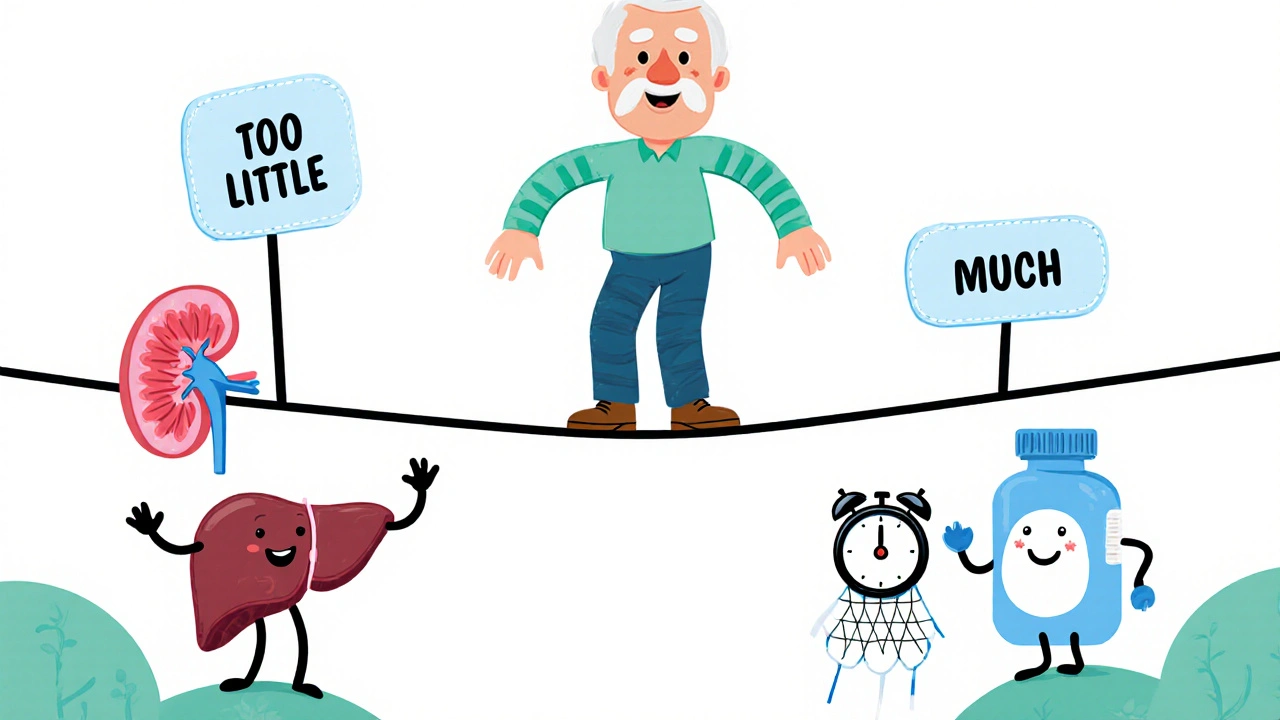
When a drug has a narrow therapeutic index, a small difference between a safe dose and a toxic one. Also known as narrow therapeutic range drugs, these medications leave almost no room for error—take too little and they don’t work; take too much and you could end up in the hospital. Think of it like walking a tightrope: one wrong step, and things go bad fast. Drugs like warfarin, digoxin, lithium, and phenytoin fall into this category. They’re used to treat serious conditions—blood clots, heart failure, seizures, bipolar disorder—but their margin for safety is razor-thin.
What makes these drugs so tricky? Their therapeutic window, the range of doses that work without causing harm is tiny. A change of just 10-20% in dosage can turn treatment into overdose. This isn’t just about pills—it’s about how your body absorbs, breaks down, and gets rid of the drug. Things like liver or kidney problems, other meds you’re taking, even what you eat can shift that balance. For example, if you’re on warfarin and start taking an antibiotic like trimethoprim, your blood can thin too much and you might bleed internally. Or if you’re on lithium and get dehydrated, your levels can spike and cause tremors, confusion, or worse.
These drugs don’t just affect patients—they challenge doctors, pharmacists, and pharmacies too. That’s why pharmacies track them closely, use special labeling, and often require regular blood tests. The medication errors, mistakes in prescribing, dispensing, or taking these drugs are among the most dangerous in healthcare. Look-alike, sound-alike names, misread prescriptions, or skipped lab tests can have life-or-death results. That’s why so many of the posts here focus on drug safety, dosing in special populations, and how to avoid mix-ups with generics or similar-looking meds.
You’re not alone if you’re taking one of these drugs. Millions of people rely on them every day. But knowing the risks isn’t enough—you need to be active in your care. Keep a symptom diary, track your doses, ask about alternatives, and never skip blood tests. If your doctor changes your dose, ask why. If you start a new supplement or over-the-counter med, check if it interacts. These aren’t just pills—they’re precision tools. Handle them right, and they save lives. Handle them wrong, and they can end them. Below, you’ll find real-world guides on how to manage these drugs safely, spot hidden risks, and avoid the mistakes that too many people make.
Adjusting Medication Dose: How to Find Your Safe and Effective Balance
Finding the right medication dose is critical for safety and effectiveness. Learn how age, kidney function, genetics, and drug interactions affect your dose-and what steps you can take to avoid dangerous side effects.
Read More