Diet for Ulcers: What to Eat and Avoid to Heal Faster
When you have a stomach ulcer, a sore in the lining of your stomach or small intestine caused by bacteria, acid, or long-term NSAID use. Also known as peptic ulcer, it’s not caused by stress or spicy food alone—but what you eat can make it worse or help it heal. The right diet for ulcers doesn’t just ease discomfort—it gives your stomach lining the chance to repair itself.
Some foods act like bandages. Bananas, for example, contain compounds that may protect the stomach lining and reduce acid. Oats and other soluble fiber sources help coat the stomach and slow digestion, lowering acid spikes. Honey, especially raw, has natural antibacterial properties that might help fight H. pylori, the main bacteria behind most ulcers. Cruciferous veggies like broccoli and cabbage have sulforaphane, a compound shown in studies to fight H. pylori. And lean proteins like chicken, fish, and tofu give your body the building blocks it needs to repair tissue without adding irritation.
On the flip side, some foods are like pouring gasoline on a fire. Coffee (even decaf), alcohol, carbonated drinks, and citrus juices crank up stomach acid. Spicy foods don’t cause ulcers, but if they make your pain worse, skip them. Fried and fatty foods delay stomach emptying, leaving acid sitting longer. And don’t forget NSAIDs like ibuprofen or aspirin—they’re common ulcer triggers. If you’re on these for pain, talk to your doctor about alternatives.
Your body doesn’t heal overnight, but what you eat every day matters more than you think. A good acid reflux diet, a way of eating that minimizes stomach acid production and irritation. Also known as low-acid diet, it overlaps heavily with ulcer-friendly eating. Small, frequent meals keep acid levels steady instead of spiking after big meals. Eating slowly gives your stomach time to process food without overworking. And never lie down right after eating—that’s when acid flows upward and burns.
People with ulcers often feel stuck between pain and hunger. But this isn’t about deprivation—it’s about smart choices. You can still enjoy meals that feel satisfying without triggering flare-ups. The goal isn’t perfection. It’s progress. Even small changes, like swapping soda for water or choosing grilled chicken over fried, can make a real difference in how you feel.
Below, you’ll find real advice from people who’ve been there—what worked, what didn’t, and how nutrition ties into medication, stress, and daily habits. No fluff. Just clear, practical tips backed by what’s been tested and proven.
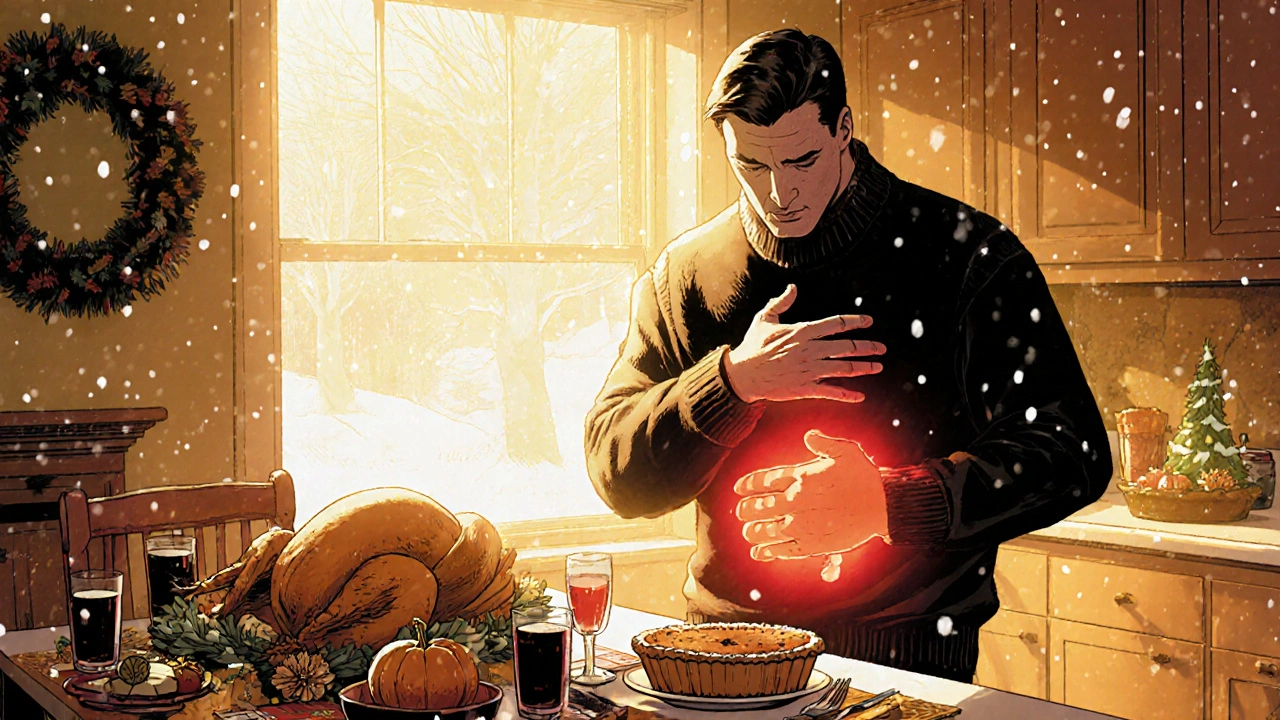
Holiday Ulcer Management: Keep Stomach Sores in Check
Learn practical steps to keep peptic ulcers under control during festive gatherings, covering diet, meds, stress, and red‑flag symptoms.
Read More