When your knee starts aching after walking just a few blocks, or your fingers feel stiff in the morning, it’s easy to think, "I’m just getting older."" But osteoarthritis isn’t normal aging. It’s a disease - and one that’s affecting over 500 million people worldwide. In the U.S. alone, 32.5 million adults have it. And for many, it’s not just discomfort - it’s lost mobility, sleepless nights, and jobs left behind.
Unlike rheumatoid arthritis, which is driven by the immune system attacking joints, osteoarthritis (OA) is about breakdown. The cartilage that cushions your bones slowly wears down. But it’s not just the cartilage. The whole joint gets involved: bone thickens, ligaments tighten, fat tissue around the joint becomes inflamed, and the lining of the joint (synovium) swells. This isn’t "wear and tear" - it’s a biological mess that turns movement into pain.
What Happens Inside Your Joint
Imagine the ends of your bones as two smooth stones sliding against each other. Between them is a layer of cartilage - soft, slippery, and full of water. It’s designed to absorb shock and let bones glide without friction. In osteoarthritis, that cartilage starts to fray. First, tiny cracks appear on the surface. Then, the collagen fibers that hold it together break apart. Chondrocytes - the cells that maintain cartilage - go into overdrive trying to repair the damage. But they can’t keep up. Instead of healing, they release chemicals that make inflammation worse.
As cartilage thins, bone starts to rub on bone. Your body tries to fix this by growing extra bone - osteophytes, or bone spurs. These can lock up your joint, making movement stiff and painful. The joint capsule stretches. Fluid builds up. Ligaments get tight. All of this adds up to one thing: pain that gets worse with activity and doesn’t fully go away with rest.
Most people think OA only hits the knees. But it’s everywhere. About 60% of cases involve the knee. Around 30% hit the hip. Hands? 25% - especially the base of the thumb and the ends of the fingers. Even the spine gets involved, with 20% of cases affecting the neck or lower back. And it’s rarely symmetrical. One knee might be fine, while the other is a mess.
Who Gets It - And Why
Age is a risk factor, yes. But 40-year-olds get OA. So do 30-year-olds. The real drivers aren’t just time - they’re load and imbalance.
Obesity is the biggest modifiable risk. Every extra pound adds 4 pounds of pressure on your knees when you walk. Losing 10% of your body weight can cut knee pain by half. That’s not a guess - it’s backed by data from the Arthritis Foundation’s surveys of 1,200 people. Those who lost weight saw real improvement. Many said they could finally climb stairs again.
Repetitive stress matters too. Construction workers have a 37% higher risk. Dancers, plumbers, and professional musicians are at higher risk too. A single serious injury - a torn ACL, a bad fracture - can lead to post-traumatic OA years later. Women are more likely to get OA than men, especially in the knees and hands. Why? Hormones, joint anatomy, and muscle strength differences all play a role.
And here’s the trap: pain makes you less active. Less activity means weaker muscles. Weaker muscles mean more stress on the joint. More stress means more damage. It becomes a loop - pain → inactivity → more pain.
What Doesn’t Work - And Why
Most people start with painkillers. NSAIDs like ibuprofen or naproxen are common. But here’s the truth: 63% of OA patients say they’re dissatisfied with these drugs. Why? Side effects. Stomach ulcers. Kidney strain. High blood pressure. And they don’t stop the disease - they just mask the pain.
Some turn to supplements. Glucosamine and chondroitin? The largest studies, including those from the NIH, show they don’t work better than placebo for most people. They’re not harmful, but they’re not magic either.
And don’t count on X-rays to catch it early. The Kellgren-Lawrence scale - used for decades - only shows damage after it’s already severe. By the time you see narrowing on an X-ray, you’ve lost 30-50% of your cartilage. That’s why experts like Dr. Virginia Byers Kraus say we need better biomarkers - blood or urine tests that detect OA before the joint is destroyed.
What Actually Works - The Real Strategies
There’s no cure. But there are ways to take control. The American College of Rheumatology says effective management needs at least three of these: weight loss, exercise, physical therapy, and education.
1. Move - Even If It Hurts
Rest won’t save your joint. Movement will. The Arthritis Foundation’s 2022 trial found that people who did land-based exercise three times a week for 45 minutes saw pain drop by 40% after 12 weeks. You don’t need to run. You don’t need a gym. Walking, cycling, water aerobics, or even tai chi help.
Why? Strong muscles around the joint - especially the quadriceps for knees - absorb shock. They take pressure off the cartilage. One study showed that people who did 150 minutes of weekly exercise improved their ability to walk 20% more than those who didn’t.
And here’s the kicker: 45% of people quit their exercise routine after six months. The key isn’t intensity - it’s consistency. Find something you don’t hate. Do it even if you’re sore. Warm up first. Cool down after.
2. Lose Weight - Even a Little
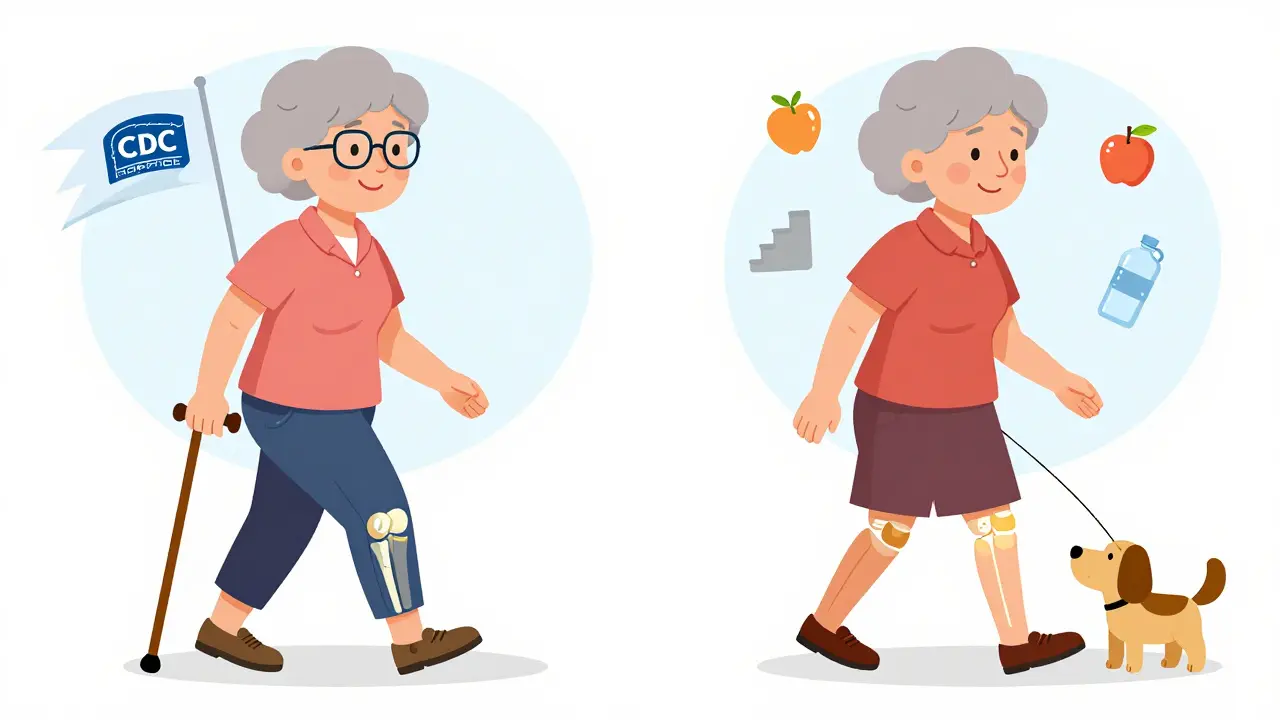
You don’t need to lose 50 pounds. Losing just 5-10% of your body weight makes a huge difference. One woman in Melbourne, 58, lost 14 pounds over six months. She went from needing a cane to walk to the store, to walking her dog daily without pain. That’s not luck - it’s biomechanics.
The CDC’s Arthritis Management Program found that people who completed a 6-week course on weight and movement reduced pain by 40% and improved function by 30%. That’s better than most medications.
3. Physical Therapy - Not Just for Injuries
Most people think PT is for post-surgery. It’s not. A certified physical therapist can teach you how to move without hurting your joint. They’ll show you how to protect your knees when you stand, how to sit without squeezing your hips, how to use your arms to take pressure off your hands.
Studies show that 6-8 sessions of PT can improve daily function more than pain meds. And unlike pills, the benefits last.
4. New Treatments on the Horizon
In June 2023, the FDA approved tanezumab - a new injection that blocks nerve growth factor. In trials, it cut pain 35% more than NSAIDs. It’s not for everyone - it’s for moderate-to-severe cases - but it’s a real step forward.
For knee OA, corticosteroid injections are now strongly recommended by OARSI. One shot can reduce pain by 50% for up to 4 weeks. It’s not a cure, but it can give you breathing room to get active.
Stem cell therapy? Still experimental. Over 387 trials are running worldwide, but no clear winner yet. Don’t pay thousands for unproven treatments. Stick to evidence.

What You Can Do Today
Here’s your simple starter plan:
- Walk for 20 minutes, three times this week. No need to push hard - just move.
- Use a step counter. Aim for 6,000 steps a day. It’s realistic. It works.
- Swap one sugary snack for fruit or nuts. Small changes add up.
- Look up your local Arthritis Foundation class. Many are free. Some even offer online sessions.
- Ask your doctor about a referral to physical therapy. Don’t wait until you’re stuck.
You don’t need to be perfect. You just need to start. And you don’t have to do it alone.
Why This Matters More Than You Think
Osteoarthritis doesn’t just hurt your joints. It hurts your life. 68% of people with OA say it interferes with sleep. 57% can’t climb stairs without help. 42% struggle with simple tasks like buttoning shirts. And 43% of working adults with OA say they’ve had to cut back on hours or change jobs.
The economic cost? $140 billion a year in the U.S. alone. But beyond money - it’s dignity. It’s independence. It’s being able to play with your grandkids, walk to the bus, or carry groceries without wincing.
What’s coming next? Blood tests that detect OA years before symptoms show up. Community programs in every state to help people move safely. Better tools for doctors to track progress.
But the biggest change? It starts with you. Not with a pill. Not with a surgery. With movement. With weight. With knowing that pain isn’t inevitable - it’s a signal. And signals can be answered.
Is osteoarthritis the same as rheumatoid arthritis?
No. Osteoarthritis (OA) is caused by mechanical wear and biological breakdown in the joint. Rheumatoid arthritis (RA) is an autoimmune disease where your immune system attacks the lining of your joints. OA pain gets worse with activity and improves with rest. RA pain is often worse in the morning and improves with movement. RA also causes swelling, fatigue, and can affect organs beyond joints.
Can you reverse osteoarthritis?
No - once cartilage is gone, it doesn’t grow back. But you can slow it down. Studies show that losing weight, exercising regularly, and doing physical therapy can stop or delay further damage. Some people even regain function and reduce pain so much that they feel like their joint is "better." It’s not cured - but it’s managed.
Do supplements like glucosamine help?
The evidence is weak. Large studies, including one by the NIH, found glucosamine and chondroitin don’t work better than a placebo for most people. Some report feeling better, but it’s likely due to placebo effect or natural symptom fluctuation. They’re generally safe, but don’t rely on them. Focus on movement and weight instead.
When should I see a doctor about joint pain?
If pain lasts more than a few weeks, gets worse with activity, wakes you up at night, or makes daily tasks hard (like climbing stairs or gripping things), it’s time. Don’t wait until you can’t walk. Early action - even just starting a walking routine or seeing a physical therapist - can change the course of the disease.
Can I still exercise if my joint hurts?
Yes - but not all exercise is equal. Avoid high-impact activities like running or jumping. Stick to low-impact options: walking, cycling, swimming, elliptical, or tai chi. Warm up first. If pain lasts more than 2 hours after exercise, you did too much. Ease back. Consistency beats intensity.
Are cortisone shots safe for osteoarthritis?
For knee OA, yes - when used appropriately. The Osteoarthritis Research Society International now recommends corticosteroid injections for flare-ups. They reduce pain by about 50% for up to 4 weeks. But they’re not a long-term fix. Limit them to 3-4 times a year. Too many can weaken tendons or cartilage over time.
Does weight loss really make a difference?
Absolutely. Losing just 10% of your body weight cuts knee pain by half in many cases. For every pound lost, you remove 4 pounds of pressure from your knees with each step. One study found that people who lost 10% of their weight improved their ability to walk 20% faster and with less pain. It’s one of the most powerful tools we have.


Post A Comment