Stress Impact on Glaucoma Calculator
Stress Level Assessment
Estimate how your stress level might impact your intraocular pressure (IOP). Enter your current stress level below and see the potential effect on your eye health.
Your Stress Impact Report
Based on your stress level () and duration ():
About This Calculation
This tool estimates how stress might affect your intraocular pressure based on research findings. It considers:
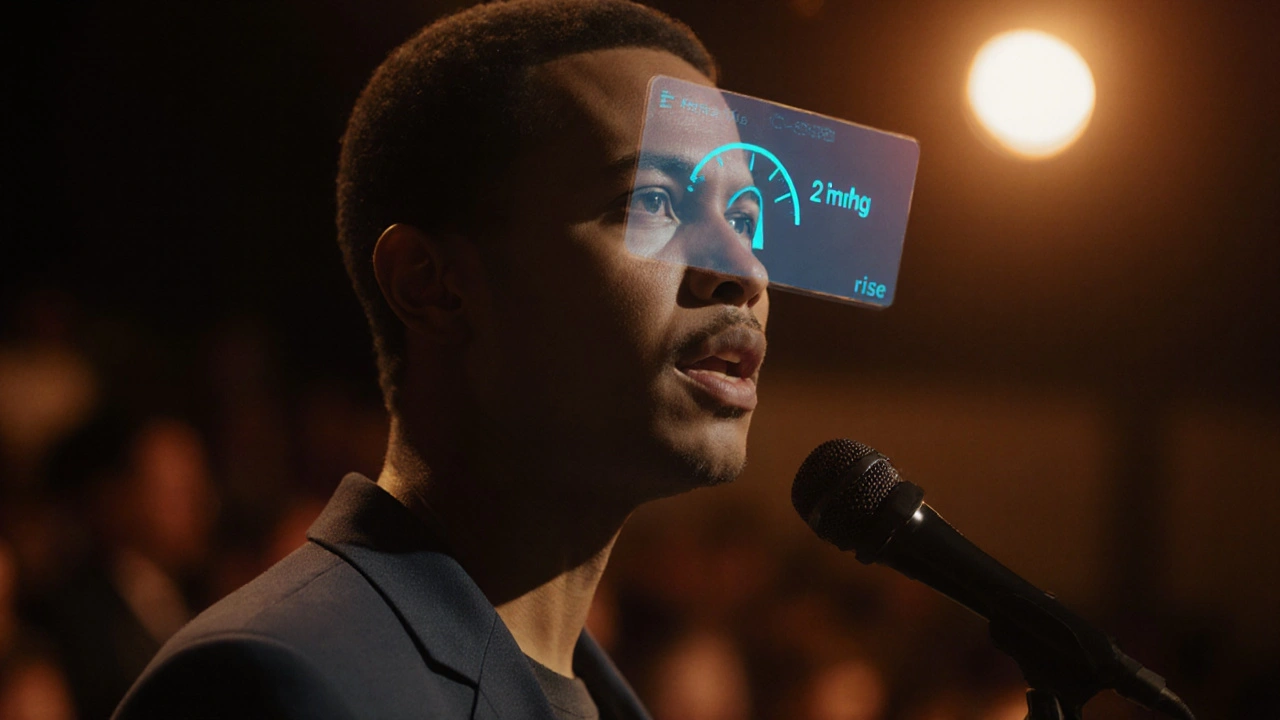
- Acute stress: Sudden spikes (e.g., public speaking) can raise IOP by 1-3 mmHg
- Chronic stress: Persistent elevation can raise baseline IOP by 2-4 mmHg
Key Takeaways
- Stress can raise intraocular pressure (IOP) and accelerate optic nerve damage.
- Elevated cortisol and blood‑pressure spikes are the main physiological links.
- Lifestyle changes-regular exercise, meditation, and sleep hygiene-help keep IOP stable.
- Monitoring stress levels is as important as tracking eye‑pressure readings for glaucoma patients.
- Consult your eye‑care professional before adding any stress‑reduction supplement or therapy.
When you hear the word Glaucoma, you probably think of eye pressure and blurry vision. What many don’t realize is that the body’s stress response can push the disease further along. Below we unpack the science, look at real‑world data, and give you practical steps to keep stress from worsening your eye health.
What Is Glaucoma?
Glaucoma is a group of eye disorders that damage the optic nerve. The nerve carries visual information from the retina to the brain, so any loss can lead to permanent vision loss. The most common form, primary open‑angle glaucoma, develops slowly and often without obvious symptoms until peripheral vision has already decreased.
The main driver of damage is elevated intraocular pressure (IOP). When fluid (aqueous humor) does not drain properly, pressure builds up, squeezing the optic nerve fibers. While high IOP is a key risk factor, genetics, age, and systemic health also play roles.
Because the disease progresses quietly, regular eye exams that measure IOP and map the visual field are the only reliable way to catch it early.
How Stress Shows Up in the Eye
Stress triggers a cascade of hormones-primarily cortisol, adrenaline, and noradrenaline. These chemicals prepare the body for “fight or flight,” raising heart rate, narrowing blood vessels, and increasing blood‑sugar levels. In the eye, the same vasoconstriction can reduce blood flow to the optic nerve while also affecting the trabecular meshwork, the tissue that drains aqueous humor.
Research shows that acute stress spikes can lift IOP by 2‑4mmHg within minutes. Chronic stress, where cortisol stays elevated for weeks or months, can lead to a sustained increase in baseline IOP, creating a perfect storm for glaucoma progression.
Stress Hormones, IOP, and Optic Nerve Damage
Let’s break down the main physiological links:
- Cortisol-High cortisol levels increase fluid retention throughout the body, including the eye, which raises IOP.
- Adrenaline-Repeated adrenaline bursts cause micro‑spasms in the tiny vessels that feed the optic nerve, reducing its oxygen supply.
- Blood Pressure-Sustained hypertension from stress adds extra force against the eye’s drainage structures, slowing fluid outflow.
When any of these mechanisms are active, the optic nerve is exposed to both mechanical pressure and a shortage of nutrients. Over time, the nerve fibers thin out, and the patient experiences visual‑field loss.
Evidence From Clinical Studies
Several studies published between 2018 and 2024 have examined stress‑related biomarkers in glaucoma patients:
- A 2020 cross‑sectional study of 312 patients found that those scoring high on the Perceived Stress Scale had an average IOP 3mmHg higher than low‑stress counterparts.
- A 2022 longitudinal trial monitored cortisol levels in 84 glaucoma patients for 12months. Participants with persistently elevated cortisol showed a 17% faster rate of visual‑field decline.
- In 2023, an eye‑pressure monitoring device recorded real‑time IOP spikes during a simulated public‑speaking event. Average IOP rose 2.8mmHg during the stress episode.
While these studies do not prove causation, the consistency across different methodologies suggests a meaningful relationship.
Practical Ways to Keep Stress From Worsening Glaucoma
Managing stress is a complement, not a replacement, for traditional glaucoma treatments (eye‑drop medications, laser therapy, or surgery). Below are evidence‑backed actions that can help keep IOP in check:
- Mind‑body practices-A 2021 meta‑analysis showed that 8‑week mindfulness programs reduced average IOP by 1.5mmHg.
- Regular aerobic exercise-Walking, cycling, or swimming for 30minutes most days improves blood flow to the optic nerve and can lower IOP by up to 2mmHg.
- Sleep hygiene-Aim for 7‑9hours per night. Poor sleep raises cortisol and has been linked to higher IOP.
- Limit caffeine-Excessive caffeine can cause short‑term IOP spikes; keep intake under 200mg per day.
- Professional counseling-Cognitive‑behavioral therapy (CBT) reduces perceived stress and has shown secondary benefits for blood‑pressure control.
When choosing a stress‑reduction technique, consider what you can stick with long term. Consistency beats intensity for hormonal balance.
Quick Checklist for Glaucoma Patients
- Schedule eye‑pressure checks at least twice a year.
- Track daily stress levels using a simple 1‑10 rating.
- Include a 10‑minute meditation or breathing exercise in your morning routine.
- Log caffeine intake and aim for a moderate amount.
- Discuss any new supplement (e.g., adaptogens) with your ophthalmologist.
Comparison Table: Stress‑Related Factors vs. Typical Glaucoma Risks
| Factor | Impact on IOP | Effect on Optic Nerve | Typical Management |
|---|---|---|---|
| Elevated cortisol (chronic stress) | +2‑4mmHg | Reduced nutrient flow, increased fiber loss | Stress‑reduction techniques, possible medication review |
| Acute adrenaline surge (e.g., public speaking) | +1‑3mmHg (temporary) | Brief optic‑nerve ischemia | Breathing exercises, avoid stimulants |
| High‑salt diet (systemic hypertension) | +1‑2mmHg | Long‑term vascular strain | Dietary changes, antihypertensive meds |
| Family history (genetic risk) | Variable | Inherent susceptibility | Early screening, regular monitoring |
| Age>60 | Gradual increase | Age‑related fiber thinning | Proactive eye‑care regimen |
Frequently Asked Questions
Can stress cause glaucoma?
Stress alone does not cause glaucoma, but it can raise intraocular pressure and accelerate optic‑nerve damage, making existing glaucoma worse.
How quickly does IOP rise during a stressful event?
Studies show a measurable rise of 2‑3mmHg within minutes of acute stress, such as a presentation or an exam.
Are there specific eye‑drop regimens for stressed patients?
The choice of drops depends on baseline IOP, not stress level. However, doctors may prescribe a more aggressive regimen if stress‑related spikes are frequent.
Is meditation enough to lower my IOP?
Meditation can lower IOP by about 1‑2mmHg in many people, which helps but should be combined with standard medical treatment.
Should I get my cortisol levels checked regularly?
If you have glaucoma and high stress, occasional cortisol testing can provide useful context, but it’s not a routine requirement for every patient.
Bottom line: while stress isn’t the root cause of glaucoma, it can tip the scales toward faster progression. By keeping stress in check, you give your eyes the best chance to stay healthy alongside any prescribed treatments.


Post A Comment