TNF Inhibitors Safety: What You Need to Know About Risks and Real-World Use
When you hear TNF inhibitors, a class of biologic drugs that block tumor necrosis factor, a protein that drives inflammation in autoimmune diseases. Also known as anti-TNF agents, they’ve changed the game for people with rheumatoid arthritis, Crohn’s disease, and psoriasis. But they’re not harmless. These drugs work by turning down your immune system’s alarm bells—and that’s where the danger starts.
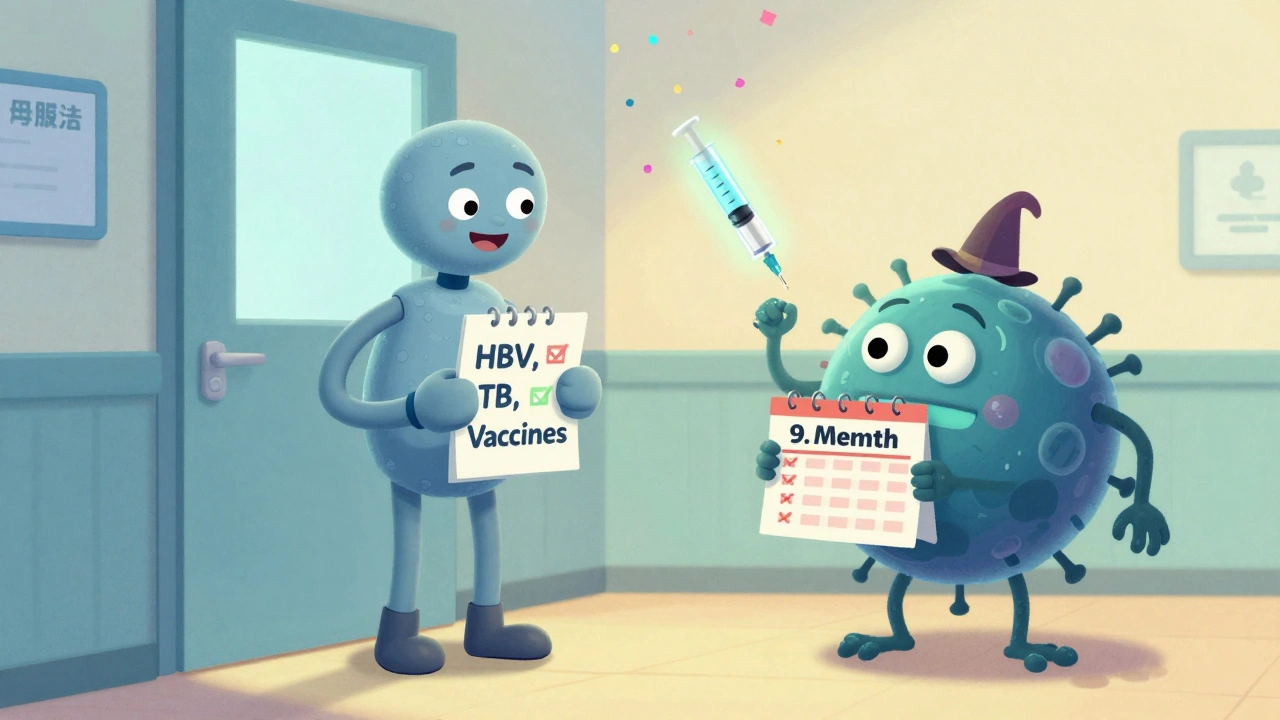
Blocking TNF helps reduce joint pain, skin plaques, and gut inflammation, but it also leaves you more open to serious infections. Tuberculosis, fungal infections like histoplasmosis, and even reactivated hepatitis B have been linked to TNF inhibitors. The FDA has issued multiple safety alerts over the years, especially for patients with a history of TB or living in areas where fungal infections are common. It’s not just about infections, either. Studies show a small but real increase in lymphoma and other cancers, especially in younger patients on long-term therapy. These aren’t theoretical risks—they show up in real patient data from the FDA’s adverse event reporting system and global pharmacovigilance databases like VigiBase.
Not everyone reacts the same way. Your age, other health conditions, and what other meds you’re taking all matter. If you’re on a TNF inhibitor and also take methotrexate or corticosteroids, your risk of infection goes up. People with heart failure, multiple sclerosis, or a history of skin cancer need extra caution. Even something as simple as a tick bite can turn serious—Lyme disease can flare or become harder to treat. That’s why doctors check for latent TB before starting treatment, and why you should never ignore a fever or unexplained fatigue while on these drugs.
There’s no one-size-fits-all answer to TNF inhibitors safety. Some people use them for years with no issues. Others have to switch after one serious side effect. The key is knowing your own risk profile and staying alert. Tracking symptoms with a simple diary—like when you feel tired, if you’ve had a fever, or if a rash shows up—can help catch problems early. And if you’re on one of these drugs, make sure your doctor knows your full medical history, including past infections, travel, and family cancer history.
What you’ll find below are real, practical guides from patients and clinicians who’ve dealt with these drugs firsthand. From how to spot early signs of infection to what alternatives exist when TNF inhibitors stop working or become too risky, these posts give you the clear, no-fluff facts you need to make smarter choices. This isn’t theory. It’s what actually happens in clinics and homes—and what you need to know to stay safe.
Biologics Safety: Infection Risk, Screening, and Vaccination Guidance for Autoimmune Patients
Biologics for autoimmune diseases reduce inflammation but increase infection risk. Learn the essential screening, vaccination, and safety steps to protect yourself before and during treatment.
Read More