Data Integrity Issues in Medications: Why Accuracy Matters for Your Health
When you take a pill, you trust that the name, dose, and instructions on the label are correct. But data integrity issues, errors or tampering in the digital or physical records that track medications. Also known as pharmaceutical data corruption, it can mean a generic drug is mislabeled, a recall notice never reaches your pharmacy, or your doctor’s system shows the wrong dosage. This isn’t theoretical—it’s happened. In 2023, the FDA flagged multiple batches of generic blood pressure pills where the active ingredient was inconsistently mixed. Patients got too much or too little. Some ended up in the ER. The problem wasn’t the drug itself—it was the pharmaceutical data, the digital and paper trails that track how a drug is made, tested, and shipped. If that data is sloppy, incomplete, or falsified, your safety depends on luck.
These issues show up in places you wouldn’t expect. A pharmacy might receive a shipment labeled as metoprolol 50mg, but the actual tablets are atenolol 50mg. The barcode scans fine, the inventory system says it’s correct, and the label looks right. But the chemical inside? Different. That’s a medication error, a preventable mistake in prescribing, dispensing, or taking a drug. And it’s often rooted in broken data. Generic drug manufacturers sometimes skip full bioequivalence testing, and the FDA’s database doesn’t catch it because the paperwork says it’s done. Or a hospital’s electronic record system auto-fills a prescription based on an old, outdated drug interaction warning—so you’re told it’s safe when it’s not. These aren’t rare glitches. They’re systemic. And they’re growing as more prescriptions move online and through automated systems.
When data integrity issues happen, the consequences aren’t just financial—they’re physical. A patient on blood thinners gets the wrong generic version because the manufacturer changed the inactive ingredients without updating the regulatory database. The drug doesn’t absorb the same way. A clot forms. Or a diabetic patient is prescribed a new insulin because the pharmacy’s system confused it with a similar-looking name. The result? A trip to the ER. These aren’t stories from a textbook. They’re real cases reported by patients and clinicians. The truth is, your health doesn’t care how clean the database looks on paper. It only cares if the right drug got to you, in the right amount, at the right time.
Below, you’ll find real-world examples of how these problems show up in everyday medications—from generic antidepressants with inconsistent potency to recalls that never reach the right people. You’ll see how drug interactions get missed because data wasn’t updated, how generic competition can hide quality gaps, and why a simple label change can have life-or-death consequences. This isn’t about blaming companies. It’s about understanding how fragile the system is—and what you can do to protect yourself.
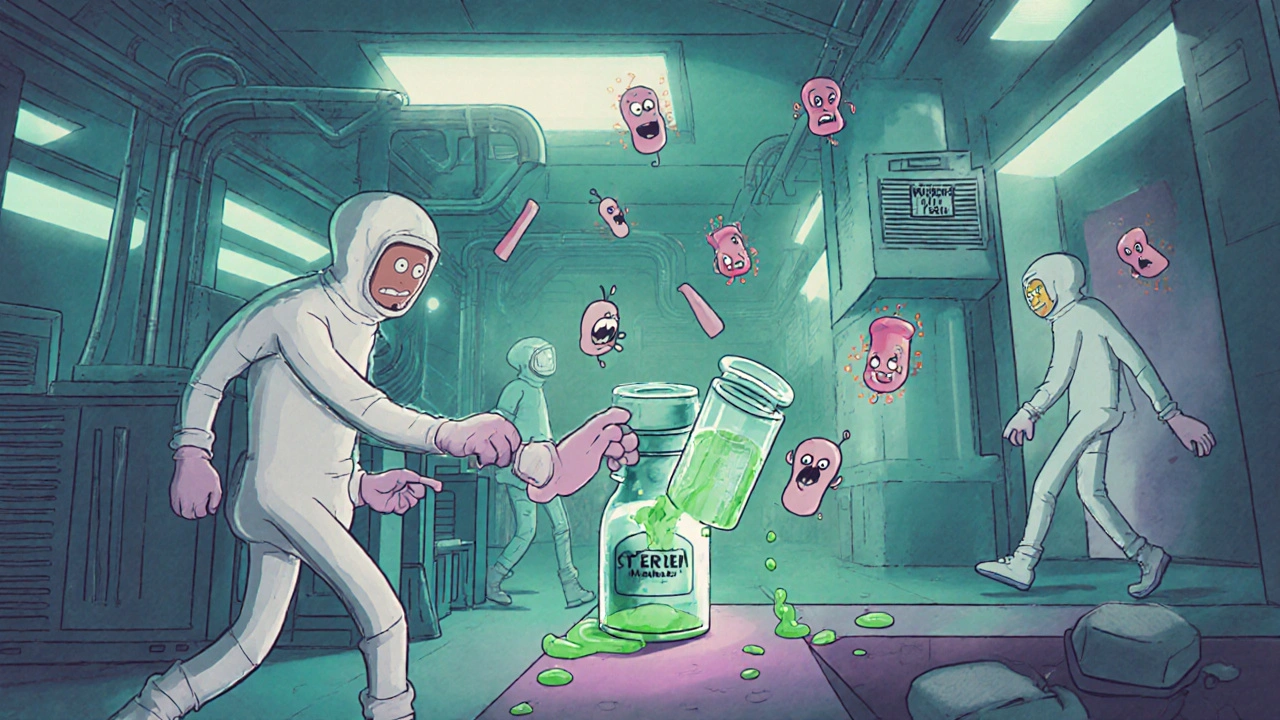
Common Manufacturing Deficiencies Found by the FDA in 2025
In 2025, the FDA issued record numbers of warning letters over manufacturing flaws like poor sterile controls, fake data, and contaminated ingredients. Learn the top 5 issues and how to avoid them.
Read More