Biologic Screening: What It Is and How It Shapes Modern Drug Safety
When you take a biologic, a complex medication made from living cells, often used for autoimmune diseases, cancer, or severe allergies. Also known as biologic therapy, it targets specific parts of your immune system with precision—but that same precision makes it harder to predict how your body will react. That’s where biologic screening, the process of testing and monitoring biologic drugs for unexpected side effects before and after they reach patients becomes critical. Unlike simple pills, biologics can trigger rare but serious immune responses, infections, or even neurological issues. Screening isn’t just a lab test—it’s an ongoing system that tracks who gets sick, when, and why.
Biologic screening ties directly into pharmacovigilance, the science and activities focused on detecting, assessing, understanding, and preventing adverse effects of medicines. Systems like VigiBase and the FDA’s MedWatch don’t just collect reports—they connect dots across thousands of patients. For example, if ten people on the same biologic for rheumatoid arthritis develop unusual nerve pain within two months, that pattern gets flagged. Screening turns scattered patient stories into actionable safety alerts. It’s how we learned that certain biologics increase tuberculosis risk, or that one drug might raise heart failure chances in older adults. This isn’t theoretical. Real people are protected because someone noticed a trend.
Biologic screening also works hand-in-hand with adverse drug reactions, harmful, unintended responses to medications at normal doses. A patient tracking symptoms in a diary? That’s screening. A pharmacist noticing a spike in reports of skin rashes after a new biologic launch? That’s screening. Even a hospital reporting a cluster of infections linked to a specific injection batch? That’s screening too. It’s not just for big pharma labs—it’s for doctors, nurses, and you. The more people report what they experience, the faster unsafe patterns are caught.
What you’ll find in these posts isn’t just theory. You’ll see real cases: how a biologic meant to calm an overactive immune system ended up triggering a dangerous infection, how a patient’s symptom diary helped uncover a hidden reaction, and how global drug safety networks flagged a risk before it became widespread. These aren’t abstract concepts. They’re stories of people who took a medication, noticed something off, and ended up helping thousands avoid the same fate. The system works when you’re part of it.
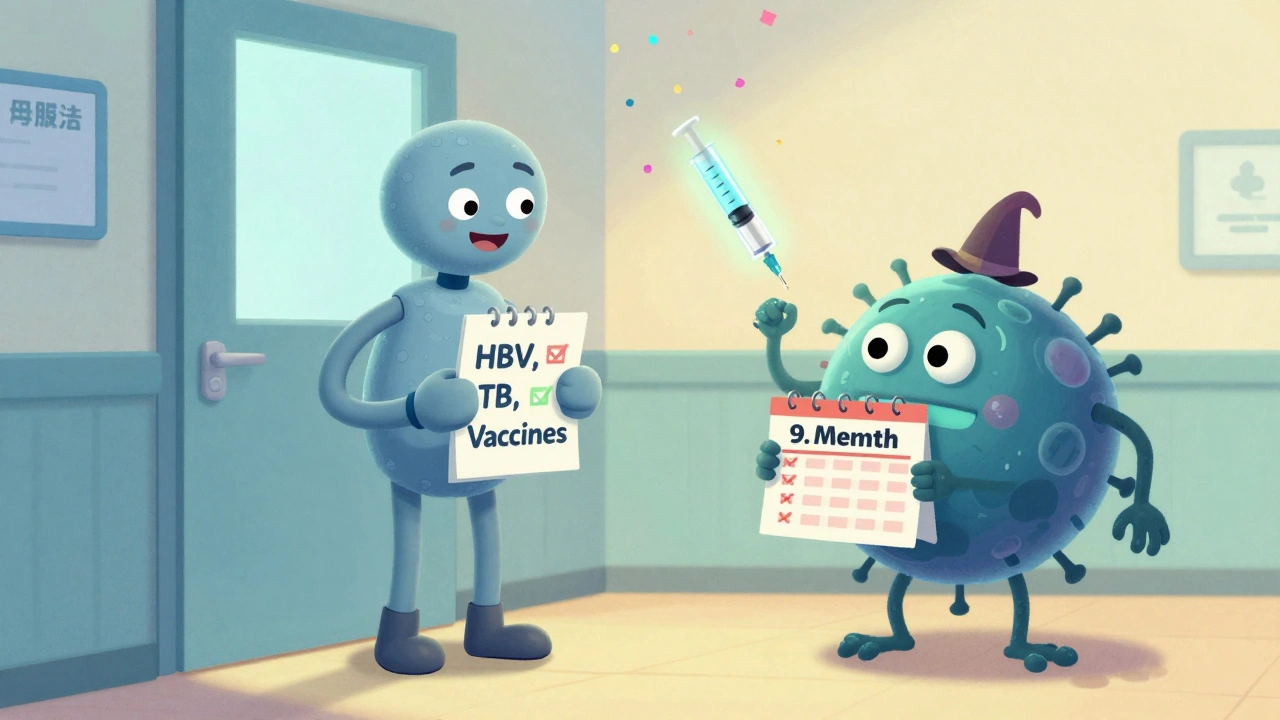
Biologics Safety: Infection Risk, Screening, and Vaccination Guidance for Autoimmune Patients
Biologics for autoimmune diseases reduce inflammation but increase infection risk. Learn the essential screening, vaccination, and safety steps to protect yourself before and during treatment.
Read More