If you’ve been living with bloating, cramps, diarrhea, or constipation that won’t go away, you’re not alone. About 1 in 7 people worldwide have irritable bowel syndrome (IBS), and for many, food is the biggest trigger-not stress, not anxiety, not some mysterious bug. The real problem? Not all diets work the same way. What helps one person makes another worse. That’s why three specific eating plans-low-FODMAP, low-residue, and elimination diets-are getting real attention from doctors and patients alike. But they’re not interchangeable. Choosing the wrong one could mean months of confusion, wasted money, or even worse symptoms.
What the Low-FODMAP Diet Really Does
The low-FODMAP diet isn’t just another gluten-free or dairy-free trend. It was created by researchers at Monash University in Melbourne, and it’s backed by over 20 clinical trials. FODMAP stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. That’s a mouthful, but it just means certain types of sugars that your gut struggles to digest. These sugars pull water into your intestines and get fermented by bacteria, causing gas, bloating, and pain.
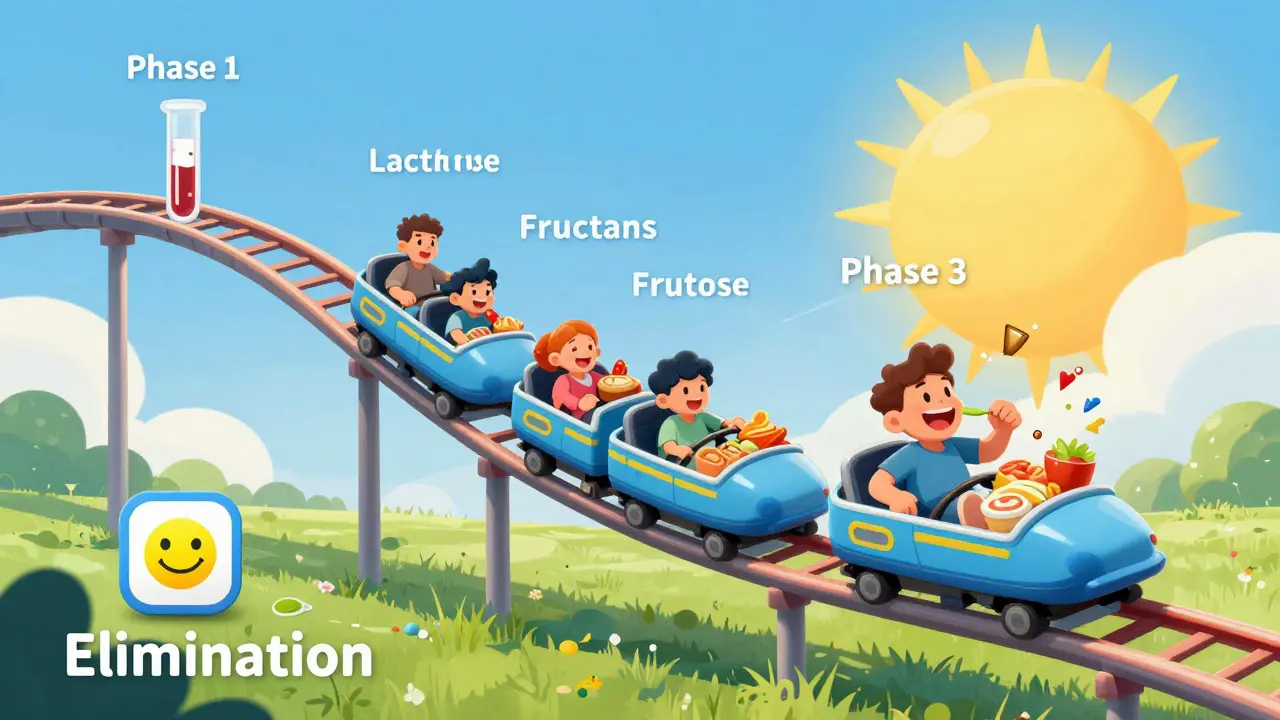
The diet has three clear phases. Phase one is strict: you cut out all high-FODMAP foods for 2 to 6 weeks. That means no garlic, onions, wheat, apples, milk, honey, or artificial sweeteners like xylitol. You eat only foods tested and certified as low in FODMAPs-things like bananas, carrots, rice, eggs, and lactose-free yogurt. Portion size matters. Even a small amount of garlic (more than 1 teaspoon) can trigger symptoms. Most people see big improvements within 10 days.
Phase two is where most people fail. You slowly bring back one FODMAP group at a time-like fructans (found in wheat and onions) or lactose (in dairy)-using precise doses. You test one group per week, eating the same amount every day for three days, while tracking symptoms. If you feel fine, you move to the next group. If you get bloated or gassy, you know that group is a trigger. Phase three is personalization. You don’t have to avoid all FODMAPs forever. Most people can tolerate small amounts of 50-80% of the foods they cut out. You’re not on a lifetime diet-you’re building a custom plan.
Studies show 75-80% of IBS patients get significant relief. One patient on Reddit said, “After 15 years of daily diarrhea, FODMAP cleared it up in three weeks.” But it’s not easy. You need the Monash FODMAP app (which costs about $50 a year) to scan barcodes and check serving sizes. Without it, you’re guessing. And if you skip phase two, you’re stuck eating boring food forever.
Low-Residue Diet: When Less Fiber Isn’t the Answer
The low-residue diet sounds simple: eat less fiber. And it’s been around since the 1940s, mostly for people with Crohn’s disease or before colon surgery. But for IBS? It’s often the wrong tool. This diet cuts fiber to 10-15 grams a day (normal intake is 25-38 grams). You avoid raw fruits and veggies, nuts, seeds, whole grains, and even legumes. Dairy is limited to lactose-free options.
It can help with diarrhea-predominant IBS by reducing stool volume. One small study found 45% of IBS patients saw less frequent bowel movements on this diet. But here’s the catch: it doesn’t touch the real problem-FODMAPs. Many low-residue foods still contain high-FODMAP ingredients. White bread? Low in fiber, but often made with wheat-full of fructans. Rice milk? Low-residue, but sometimes sweetened with agave (high in fructose).
Long-term, this diet is risky. Folate levels drop by 35%, calcium by 25%. You’re more likely to get constipated, especially if you have constipation-predominant IBS. And you’re missing out on prebiotics that feed good gut bacteria. A 2022 analysis from the Canadian Digestive Health Foundation found that 60-70% of IBS patients don’t need this level of fiber restriction. If you’re not under a dietitian’s care, you’re just making your gut weaker.
General Elimination Diets: The Wild West of IBS Eating
Elimination diets are the DIY version of FODMAP. You cut out common triggers-dairy, gluten, caffeine, eggs, soy-for 2-4 weeks, then add them back one at a time. Sounds logical, right? But without structure, it’s a mess.
Unlike FODMAP, there’s no standard dosing. You don’t know if you’re eating 1 gram or 10 grams of lactose. You might cut out gluten because you think it’s the culprit, but your real trigger is onions in your soup. A 2023 study from the University of Virginia found that only 30% of people correctly identify their trigger foods without professional guidance. That means 7 out of 10 people are eliminating foods they don’t need to, while still eating the ones that hurt them.
It’s also less specific. FODMAP targets only five types of sugars. Elimination diets might remove 10-15 food groups. That’s harder to follow, harder to reintroduce, and more likely to cause nutrient gaps. If you’re doing this on your own, you’re gambling with your nutrition.
Still, it has a place. If you can’t access a dietitian or can’t afford the Monash app, starting with an elimination diet is better than doing nothing. Just don’t stop there. If symptoms improve, get tested properly. You deserve more than guesswork.
Which Diet Is Right for You?
Here’s how to pick:
- Choose low-FODMAP if you have bloating, gas, abdominal pain, or mixed diarrhea/constipation. It’s the only diet proven to target the root cause of IBS symptoms in most people.
- Try low-residue only if you have severe, frequent diarrhea and your doctor recommends it for short-term relief (like before a procedure). Don’t use it long-term.
- Use elimination diets as a starting point if you have no access to FODMAP resources-but only if you plan to upgrade to a structured plan later.
One big mistake? Starting all three at once. That’s like trying to solve a math problem by changing every number. You won’t know what helped. Stick to one plan at a time.
Also, if you have a history of eating disorders, avoid the low-FODMAP diet. The restrictions can trigger unhealthy behaviors. Talk to your doctor first.
How to Actually Do This Without Losing Your Mind
Here’s what works in real life:
- Get the Monash FODMAP app. It’s not optional. It tells you exact serving sizes and which foods are safe. The barcode scanner saves hours.
- Meal prep for 4 days. Cook rice, grilled chicken, steamed carrots, and lactose-free yogurt in bulk. Keep it simple.
- Track symptoms daily. Use a notebook or free app. Note what you ate, when you ate it, and how you felt 2-24 hours later.
- Don’t skip reintroduction. This is where the magic happens. You’re not trying to stay on phase one forever.
- Find a certified dietitian. Look for one trained in FODMAP through Monash University’s directory. Even one session can save you months of trial and error.
Many people think they have to give up eating out. You don’t. Learn to ask: “Is there garlic or onion in this?” “Is the sauce made with honey or agave?” Carry a FODMAP-friendly restaurant card. Most places will accommodate you.
What No One Tells You About FODMAP
Yes, it works. But it’s not a cure. It’s a management tool. Your gut doesn’t magically heal-you’re just avoiding the triggers that make it scream.
During phase one, your gut bacteria change. Bifidobacterium, a good bacteria, drops by 40% in four weeks. That’s why reintroduction is critical. You need to feed your gut the right fibers again-just not the ones that hurt you.
Also, not everyone responds. About 20-25% of IBS patients don’t improve on FODMAP. That doesn’t mean you failed. It means your triggers might be something else-like bile acid malabsorption, small intestinal bacterial overgrowth (SIBO), or even stress. Talk to your doctor about other tests.
And yes, it’s expensive. The app, the low-FODMAP foods, the dietitian-add up. But compare that to years of doctor visits, medications, and missed work. This is an investment in your quality of life.
What’s Next for IBS Diets?
Science is moving fast. Monash University just updated its app with AI meal planning and 1,200 new foods. Researchers are testing blood and stool biomarkers to predict who will respond to FODMAP before they even start. By 2026, your doctor might be able to pull your FODMAP response data right from your electronic health record.
For now, stick with what’s proven. The low-FODMAP diet is the gold standard-not because it’s trendy, but because it’s precise, personal, and backed by real data. It’s not perfect. But it’s the best tool we have.
Don’t settle for vague advice. Don’t trust random blogs. If you have IBS, you deserve a plan built on science-not guesswork.
Can I do the low-FODMAP diet without the app?
You can try, but you’re likely to make mistakes. Many foods have hidden FODMAPs-like soy sauce, protein bars, and even some ‘healthy’ snacks. The Monash FODMAP app uses lab-tested serving sizes and updates its database regularly. Without it, you might eat too much of a ‘low-FODMAP’ food and trigger symptoms. It’s not just a tool-it’s your safety net.
Is the low-residue diet safe for long-term use?
No. Long-term use leads to nutrient deficiencies, especially in folate, calcium, and fiber. It can worsen constipation and starve your gut bacteria. It’s meant for short-term relief, like before surgery or during a flare-up. For ongoing IBS management, it’s not appropriate for most people.
Why do some people get worse during FODMAP reintroduction?
It’s normal. When you reintroduce FODMAPs, your gut is adjusting. Symptoms like bloating or gas can flare up as your body reacts to the sugars. That doesn’t mean you’re doing it wrong-it means you’re learning. The key is to track symptoms carefully and only reintroduce one group at a time. If symptoms are severe, pause for a few days and try again later with a smaller dose.
Can I eat out on a low-FODMAP diet?
Yes, but you need to plan. Choose simple dishes: grilled chicken or fish with steamed vegetables and rice. Avoid sauces, dressings, and soups unless you know the ingredients. Ask if garlic or onion is used. Many restaurants are used to dietary requests now. Carry a FODMAP-friendly card from Monash University-it makes communication easier.
How long does the whole FODMAP process take?
The full process usually takes 3 to 6 months. Phase one (elimination) lasts 2-6 weeks. Phase two (reintroduction) takes 8-12 weeks. Phase three (personalization) is ongoing. Most people feel better within the first month, but the real goal is to find your personal tolerance-not to stay restricted forever.
What if the low-FODMAP diet doesn’t work for me?
You’re not alone. About 1 in 4 people don’t respond. That doesn’t mean you’re broken-it means your IBS might be driven by something else: bile acid issues, SIBO, stress, or even food intolerances outside FODMAPs. Talk to your doctor about other tests. You might need a different approach, like a low-fat diet, peppermint oil, or gut-directed hypnotherapy.


Post A Comment