Every year, thousands of people in Australia and around the world take the wrong medication-not because they’re careless, but because the label on their pill bottle was wrong. A pharmacy technician meant to fill your blood pressure medicine, but handed you a diabetes drug instead. The strength says 5 mg, but it should’ve been 0.5 mg. The name looks almost the same: glipizide instead of glyburide. And you didn’t notice until it was too late.
You’re not alone. Studies show that about 1 in 5 medication errors happen at the pharmacy counter. Even the best pharmacists make mistakes. That’s why the final check isn’t theirs-it’s yours. Before you swallow that pill, take 90 seconds to verify the label. It could save your life.
What to Check on Every Prescription Label
Don’t just glance at the bottle and assume it’s right. Read it like you’re reading a warning sign on a machine. There are five critical pieces of information you must confirm every single time:
- Drug name (both brand and generic)
- Strength (how much is in each pill or dose)
- Dosage form (tablet, capsule, liquid, patch)
- Directions for use (how often, when, with or without food)
- Indication (why you’re taking it)
Most pharmacy labels skip the indication. That’s a problem. If your label says “Take one tablet daily” but doesn’t say it’s for high blood pressure, you might not realize you’ve been given a completely different drug. A 2016 study found that when the reason for the medication was printed on the label, patients caught 63% more errors. Always ask for it. If it’s not there, say so.
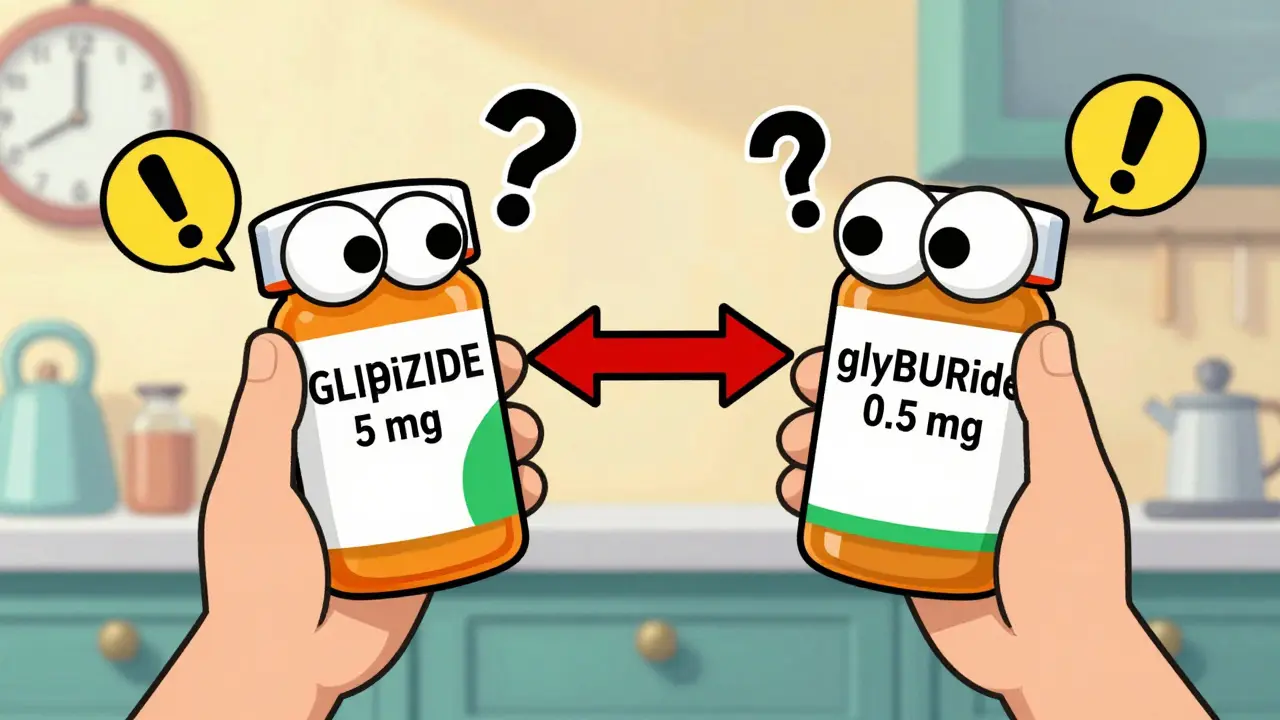
Watch Out for Look-Alike, Sound-Alike (LASA) Drugs
Some drug names are dangerously close. One letter, one syllable, one typo-and you’re at risk. These are called look-alike, sound-alike (LASA) errors. They account for nearly 30% of all dispensing mistakes.
Here are real examples that have caused serious harm:
- Glipizide (for diabetes) vs. glyburide (also for diabetes-but different dose, different risk)
- Hydralazine (for high blood pressure) vs. hydroxyzine (for anxiety and allergies)
- Cycloserine (for tuberculosis) vs. cyclosporine (for organ transplant patients)
Pharmacies are supposed to use tall-man lettering to highlight the differences: GLIpiZIDE vs. glyBURide. But only about 30% of community pharmacies do it consistently. Don’t wait for them to fix it-look for it yourself. Read the name slowly. Say it out loud. If it sounds like another medicine you’ve taken before, pause. Double-check.
Decimal Points and Zeros Can Kill
One misplaced decimal point turns a safe dose into a deadly one. This isn’t rare. It happens more often than you think.
Take warfarin, a blood thinner. The right dose might be 0.5 mg. If the label says 5 mg? That’s ten times too much. One dose can cause internal bleeding. Levothyroxine, used for thyroid problems, has the same risk. A 0.025 mg error can throw your whole metabolism off.
Here’s how to catch it: Read the numbers aloud. Say “zero point five milligrams,” not “point five.” If you say “five milligrams” and it doesn’t sound right, stop. Compare it to your last prescription. Did you used to take 0.5 mg? Then why is this one 5 mg? Ask the pharmacist to confirm.

Compare to Your Last Bottle
Don’t just trust the new label. Hold it next to the last one you had. Even if it’s the same drug, check for changes.
Did the color change? The shape? The imprint code on the tablet? Did the directions go from “once daily” to “twice daily”? Did the pill size suddenly get bigger or smaller? These are red flags.
A 2021 study found that patients who compared their new prescription to their old one caught 89% of errors. Those who just glanced at the new label? Only 42%. That’s not luck-it’s a system. Make it part of your routine. Keep your old bottles for at least a week after starting a new one. Take a photo of the label if you’re worried about forgetting.
High-Alert Medications Need Extra Care
Some drugs are more dangerous if given wrong. These are called “high-alert medications.” If you’re taking one, treat the label like a bomb squad checklist.
The top three are:
- Insulin (wrong dose = coma or death)
- Anticoagulants like warfarin or apixaban (wrong dose = stroke or bleeding)
- Opioids like oxycodone or morphine (wrong dose = respiratory failure)
These account for 65% of all serious labeling errors. If you’re on any of these, don’t skip the verification. Ask the pharmacist to explain why you’re taking it. Repeat it back. If they seem annoyed, that’s not your problem. Your life is.
Use Technology-But Don’t Rely on It
There are apps now that can scan your label and compare it to your prescription. CVS has a feature called “Label Lens” that lets you scan a QR code and hear an audio description of your medication. Apps like MedSafety Check use your phone’s camera to match the label to the expected drug with 95% accuracy.
But here’s the catch: technology can’t replace your brain. If you’re told your pill is “metformin 500 mg” but your doctor said “1000 mg,” the app might not catch it if the label says the wrong thing. It only compares what’s on the label to what’s in the system. If the system has the wrong data? So does the app.
Use tech as a second pair of eyes-not your only one. Always read the label yourself first.
Why People Don’t Check-And Why They Should
Most people don’t verify their labels because they trust the pharmacy. That’s understandable. Pharmacists are trained professionals. But trust isn’t a safety system. It’s a hope.
A 2022 survey found that 58% of people who never check their labels said they trusted the pharmacy. Another 32% said they didn’t know what to look for. That’s the gap we’re trying to close.
Here’s the truth: Pharmacists are overworked. In community pharmacies, they’re often filling 200+ prescriptions a day. Mistakes happen. The 2020 Institute of Medicine report made it clear: the final safety check isn’t the pharmacist’s job-it’s yours.
You’re not being difficult. You’re being smart.
What to Do If You Find a Mistake
Don’t panic. Don’t take the medication. Don’t throw it away.
Call the pharmacy. Say: “I’m checking my prescription. The label says [what it says], but my doctor prescribed [what it should be]. Can you please confirm this is correct?”
Be polite, but firm. If they say, “Oh, that’s right,” and you’re still unsure, ask to speak to the pharmacist directly. If they dismiss you, go to another pharmacy and get it filled there. Bring the original label with you.
If you’ve already taken the wrong dose, call your doctor or go to the emergency room. Don’t wait. Write down what you took, when, and what you’re feeling. That information could save your life.
Final Reminder: 90 Seconds Can Save You
It takes less than two minutes to check your label properly. Compare the name. Read the strength out loud. Check the form. Confirm the reason. Look for tall-man letters. Compare to your last bottle.
You wouldn’t drive a car without checking the brakes. Don’t take a pill without checking the label. Medication errors are preventable. But only if you’re the one who catches them.
That’s your power. That’s your responsibility. And that’s how you stay safe.

Post A Comment