When your liver starts to scar, it’s not just a minor issue-it’s a warning that your body is fighting a slow, silent battle. Cirrhosis isn’t a single disease. It’s the end result of years of damage, where healthy liver tissue gets replaced by stiff, useless scar tissue. By the time most people find out they have it, the damage is already done. But here’s the thing: cirrhosis doesn’t have to be a death sentence. If caught early, you can still stop it from getting worse. And if it’s advanced, a transplant can give you a second chance.
What Happens When Your Liver Turns to Scar Tissue
Your liver is one of the toughest organs in your body. It filters toxins, makes proteins, stores energy, and helps digest food. But it can only take so much abuse. Every time it’s damaged-by alcohol, hepatitis, or fat buildup-it tries to heal itself. That healing process creates scar tissue. Normally, that’s fine. But if the damage keeps coming, the scars pile up. And soon, they start to crowd out the healthy cells. This isn’t just about stiffness. Scar tissue blocks blood flow through the liver. That raises pressure in the portal vein, which brings blood from your intestines to your liver. When that pressure gets too high, fluid leaks into your belly-called ascites. It can also cause veins in your esophagus to swell and burst, leading to dangerous bleeding. Your liver stops making enough albumin, so you swell up. Your blood doesn’t clot right. Your brain gets foggy from toxins it can’t filter out. The scary part? You might feel fine until it’s too late. That’s why cirrhosis is often called a silent disease. Many people don’t have symptoms until their liver is barely working. A routine blood test showing high liver enzymes or low platelets can be the first clue.Compensated vs. Decompensated: The Two Stages That Change Everything
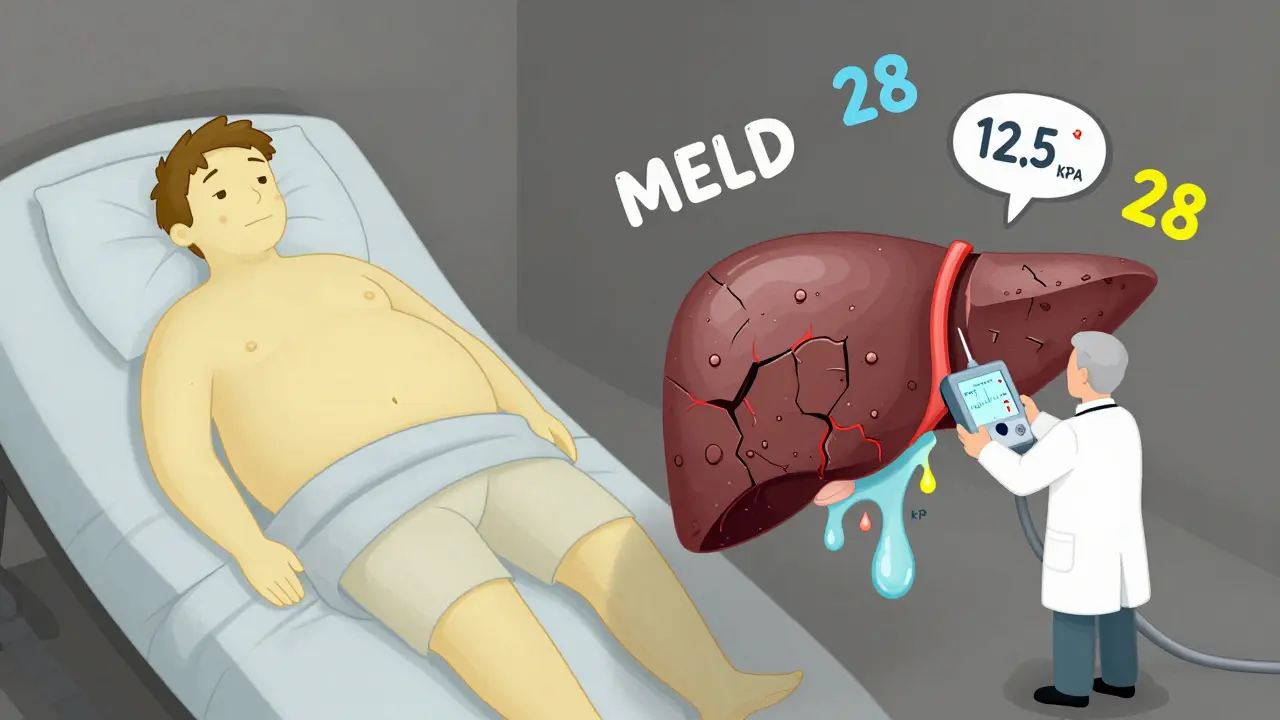
Not all cirrhosis is the same. Doctors split it into two stages: compensated and decompensated. That difference decides your survival odds. In compensated cirrhosis, your liver is scarred, but it’s still doing enough to keep you alive. You might feel tired, or have mild discomfort, but you’re not in crisis. About 80-90% of people in this stage survive five years or more. The goal here is simple: stop the damage. Quit drinking. Get treated for hepatitis C. Lose weight if you have fatty liver. If you do that, your liver can sometimes stabilize. Some early scarring can even improve. Decompensated cirrhosis is where things turn dangerous. Your liver can’t keep up anymore. You develop complications: fluid in your belly, bleeding from swollen veins, confusion from toxin buildup (hepatic encephalopathy), or jaundice-your skin and eyes turning yellow. At this point, your 5-year survival drops to 20-50%. No medication can reverse this. The only real option left is a transplant. The MELD score-ranging from 6 to 40-is used to rank how sick you are. A score above 15 means you’re at high risk of dying within a year without a transplant. A score over 25? You’re in urgent need.What Causes Cirrhosis? The Top Three Culprits
Cirrhosis doesn’t come out of nowhere. It’s the end of a long road of damage. In the U.S., three causes make up most cases:- Alcohol-related liver disease: Even if you don’t consider yourself a heavy drinker, daily drinking over years can destroy your liver. One drink a day for 10-15 years is enough to start scarring.
- Non-alcoholic fatty liver disease (NAFLD): This is now the fastest-growing cause. It’s tied to obesity, diabetes, and high cholesterol. What starts as fat buildup turns into inflammation, then scarring. It’s silent, sneaky, and often missed until it’s advanced.
- Hepatitis C: Once the leading cause, it’s now less common thanks to new antiviral drugs. But many people were infected decades ago and didn’t know it. Today, most cases are diagnosed late-when cirrhosis is already present.
How Is Cirrhosis Diagnosed? No Need for a Knife Anymore
Years ago, the only way to confirm cirrhosis was a liver biopsy-a needle stuck through your skin to pull out a tiny piece of liver. It was painful, risky, and not always accurate. Now, doctors use non-invasive tools that are faster, safer, and just as reliable. The most common is transient elastography, also called FibroScan. It uses sound waves to measure how stiff your liver is. A reading above 12.5 kPa strongly suggests cirrhosis. Blood tests also help-low albumin, high bilirubin, high INR, low platelets. Imaging like ultrasound or MRI can show liver texture changes and signs of fluid buildup. A 2023 study in the Journal of Hepatology found that MRI elastography is even more accurate than FibroScan, hitting 90% accuracy. But FibroScan is still the go-to because it’s cheaper and widely available. The key? Don’t wait for symptoms. If you have risk factors-obesity, heavy drinking, hepatitis, diabetes-get checked. A simple scan can save your life.Can Cirrhosis Be Reversed? The Hard Truth
Here’s what most people want to know: Can I fix this? The answer is: only if it’s early. In compensated cirrhosis, removing the cause-like stopping alcohol or curing hepatitis C-can slow or even reverse some scarring. Studies show that up to 20% of patients with early-stage cirrhosis from hepatitis C see fibrosis improve after successful treatment. But once you’re in decompensated cirrhosis? No pill, no supplement, no diet will undo the damage. The scar tissue is permanent. That’s why prevention and early detection are everything. There’s hope on the horizon. New drugs in clinical trials, like simtuzumab, are targeting the actual scarring process. Early results show a 30% reduction in fibrosis progression in fatty liver-related cirrhosis. But these aren’t available yet. For now, the only cure for advanced cirrhosis is a transplant.
Liver Transplant: The Last Resort That Saves Lives
If your liver is failing, a transplant is your best shot. It’s not easy. You have to be healthy enough to survive surgery. You need to prove you’ve stopped drinking or managing your weight. You need a support system. And you need to wait. In the U.S., about 14,300 people are on the liver transplant waiting list. Only 8,780 transplants were done in 2022. That means roughly 12% of people on the list die each year waiting. The system uses MELD-Na scores to decide who gets priority. The sicker you are, the higher your rank. It’s cold, but fair. Someone with a MELD score of 35 gets a liver before someone with a score of 18. Transplant success rates are high-over 85% survive one year, and 75% survive five years. But it’s not a cure-all. You’ll need to take anti-rejection drugs for life. You’ll need regular checkups. And you’ll still be at risk for other health problems. New tech is helping. Machines that keep donor livers alive and warm during transport-called normothermic perfusion-have increased the number of usable livers by 22%. That means more people get transplants faster.Living With Cirrhosis: Daily Realities No One Talks About
If you’re living with cirrhosis, your life changes in ways you didn’t expect. You’ll need to eat less salt-under 2,000 mg a day. That means no processed food, no canned soup, no soy sauce. You’ll need to track protein intake. Too much can worsen brain fog. Too little can make you weak. You’ll monitor your weight every day. A two-pound gain in 24 hours? That could mean fluid is building up. You’ll learn to recognize the signs of confusion-forgetting names, slurred speech, hand tremors. Those are red flags for hepatic encephalopathy. Many people report chronic fatigue that no amount of sleep fixes. One Reddit user wrote: “Even after my transplant, the mental fog took six months to clear.” Support matters. The American Liver Foundation offers nurse navigation services. Multidisciplinary clinics-where hepatologists, dietitians, and social workers work together-cut hospital visits by 40% in alcoholic cirrhosis patients. But access is uneven. Only 35% of rural U.S. counties have a liver specialist. If you’re in a small town, you might be traveling hours for care.What’s Next? The Future of Cirrhosis Care
The field is changing fast. Researchers are moving beyond just staging cirrhosis by MELD or Child-Pugh scores. They’re starting to look at molecular signatures-specific proteins and genes that tell you how aggressive your scarring is. That could lead to personalized treatments. Bioartificial livers-devices that temporarily take over liver function-are in early human trials. Stem cell therapies are being tested to regenerate liver tissue. One 2023 study showed a 40% drop in MELD scores after hepatocyte transplantation. But the biggest challenge remains: organ shortage. Until we solve that, transplants will remain a lottery. Public awareness needs to rise. More people need to register as donors. More funding needs to go into research. For now, the best strategy is simple: protect your liver before it’s too late. If you’re at risk, get tested. If you have cirrhosis, follow your plan. And if you’re told you need a transplant-don’t wait. The clock is ticking.Can you live a normal life with cirrhosis?
Yes-but only if it’s caught early. In compensated cirrhosis, many people live for years with few symptoms, as long as they avoid alcohol, manage their weight, and follow their doctor’s advice. Once cirrhosis becomes decompensated, daily life becomes much harder. You’ll need frequent medical visits, strict diet changes, and may require hospitalizations. Quality of life drops significantly, but a successful transplant can restore it.
Is cirrhosis always caused by alcohol?
No. While alcohol is a major cause, non-alcoholic fatty liver disease (NAFLD) is now the leading cause in the U.S., especially among people with obesity or type 2 diabetes. Hepatitis C, autoimmune diseases, and genetic conditions also cause cirrhosis. In fact, nearly half of all cirrhosis cases in the U.S. are not related to alcohol.
How do you know if your cirrhosis is getting worse?
Watch for new or worsening symptoms: swelling in your belly or legs, yellowing of skin or eyes, confusion or memory problems, vomiting blood, or extreme fatigue. Sudden weight gain (more than 2 pounds in a day) often means fluid buildup. If you notice any of these, contact your doctor immediately. Regular blood tests and imaging also track progression.
Can a liver transplant cure cirrhosis?
A transplant replaces the damaged liver with a healthy one, effectively curing the cirrhosis. However, the underlying cause must be addressed. For example, if you had alcoholic cirrhosis, you must stay sober for life. If you had fatty liver disease, you must maintain a healthy weight. The transplant fixes the organ, but not the behavior that caused the damage.
Are there any new drugs to treat cirrhosis?
There are no drugs yet that can reverse advanced cirrhosis. But new treatments are in development. Obeticholic acid is approved for certain bile duct diseases that lead to cirrhosis. Drugs like simtuzumab, which target fibrosis directly, are in phase 3 trials and show promise in slowing progression. These aren’t cures, but they may delay the need for a transplant.


Post A Comment