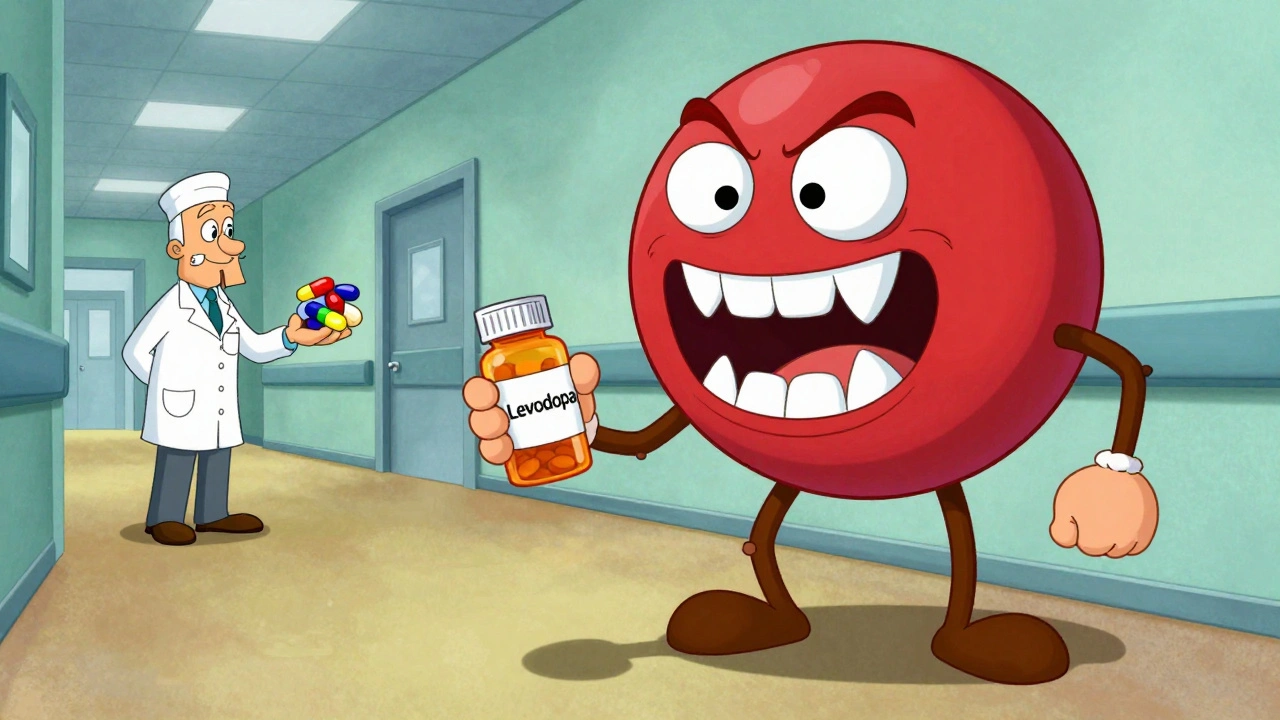
When you’re living with Parkinson’s disease, nausea isn’t just an inconvenience-it’s a common side effect of your life-saving medication. Levodopa, the gold standard treatment, triggers nausea in 40% to 80% of patients, especially when starting therapy. But here’s the catch: the very drugs doctors reach for to stop that nausea-like metoclopramide or prochlorperazine-can make your Parkinson’s symptoms worse. That’s not a rare mistake. It’s a well-documented, preventable crisis in patient care.
Why Dopamine Blockers Are Dangerous for Parkinson’s Patients
Parkinson’s disease is caused by the slow death of dopamine-producing neurons in the brain. That’s why patients take levodopa: to replace what’s been lost. But antiemetics like metoclopramide, haloperidol, and prochlorperazine work by blocking dopamine receptors. If those drugs get into the brain, they don’t just stop nausea-they also block the dopamine your body is desperately trying to restore. This isn’t theoretical. It’s clinical reality. Patients report sudden worsening of tremors, freezing episodes, and stiffness after receiving these drugs in emergency rooms or after surgery. One patient on the Parkinson’s NSW Forum described how a single dose of metoclopramide after dental surgery sent his tremors into overdrive. It took three weeks to recover, even after increasing his levodopa dose. The problem isn’t just about feeling worse. It’s about safety. Dopamine antagonists can trigger acute dystonia, delirium, and even neuroleptic malignant syndrome-a rare but deadly condition. The Michael J. Fox Foundation’s 2022 patient survey found that 68% of Parkinson’s patients who received dopamine-blocking antiemetics in hospital saw a sharp decline in motor function. Over 20% needed extended hospital stays.The Big Three: Metoclopramide, Prochlorperazine, and Haloperidol
These three drugs are the most common offenders. They’re cheap, widely available, and often the first choice in hospitals for nausea. But for Parkinson’s patients, they’re dangerous.- Metoclopramide (Reglan, Maxalon): Even though it’s used to treat gastroparesis and nausea, it crosses the blood-brain barrier and blocks dopamine receptors. The American Parkinson Disease Association lists it as one of the top medications to avoid. Despite this, it’s still prescribed to Parkinson’s patients-often by doctors who don’t know the risk.
- Prochlorperazine (Stemetil): Used for vertigo and nausea, this phenothiazine is a potent dopamine blocker. Parkinson’s UK explicitly warns against its use. Patients on forums report severe ‘off’ periods after even one dose.
- Haloperidol (Haldol): An antipsychotic, but sometimes used off-label for nausea. It’s one of the most dangerous options. It can cause irreversible movement disorders and is strictly contraindicated in Parkinson’s.
The risk isn’t just theoretical. A 2022 study in the Journal of Parkinson’s Disease found that only 37% of emergency physicians could correctly identify metoclopramide as unsafe for Parkinson’s patients. That means over 60% of the time, the person deciding your treatment doesn’t know the danger.
Safer Alternatives: What Actually Works
There are effective antiemetics that don’t touch dopamine receptors. You don’t have to suffer through nausea or risk worsening your condition.- Domperidone (Motilium): This is the gold standard for Parkinson’s patients. It blocks dopamine in the gut, where it stops nausea, but can’t cross the blood-brain barrier thanks to P-glycoprotein pumps. Studies show less than 2% risk of worsening motor symptoms. The catch? It’s not available as an injection in the U.S. and requires special approval from the FDA due to heart rhythm concerns-though those risks are minimal at standard doses.
- Cyclizine (Vertin): An antihistamine that works on H1 receptors, not dopamine. It’s been shown to be effective for nausea with only a 5-10% risk of worsening Parkinson’s symptoms. One Reddit user switched from metoclopramide to cyclizine and said, “The difference was night and day-no more freezing episodes.”
- Ondansetron (Zofran): Blocks serotonin (5-HT3) receptors. It’s safe for dopamine pathways, with only 15-20% risk of interaction. But it’s less effective for nausea caused by delayed gastric emptying, which is common in Parkinson’s.
- Levomepromazine (Nozamine): A middle-ground option. It has some dopamine-blocking activity but is sometimes used in palliative care. Only under specialist supervision, and at the lowest possible dose (6.25-25 mg daily).
- Aprepitant (Emend): A newer option that blocks neurokinin-1 receptors. A 2023 trial with 120 Parkinson’s patients showed 92% effectiveness for nausea with zero worsening of motor symptoms. It’s expensive and not yet widely used, but it’s a promising future option.

Non-Drug Strategies That Work
Before reaching for a pill, try these simple, proven methods:- Ginger: 1 gram daily (in capsule, tea, or fresh form) has been shown in multiple studies to reduce nausea without side effects.
- Small, frequent meals: Large meals delay gastric emptying and worsen nausea. Eating five small meals a day helps.
- Stay hydrated: Dehydration makes nausea worse. Sip water or electrolyte drinks throughout the day.
- Timing your levodopa: Take it on an empty stomach, at least 30 minutes before or 60 minutes after meals. Protein interferes with absorption and can trigger nausea.
- Posture: Sit upright for 30-60 minutes after eating. Lying down slows digestion and increases reflux.
Dr. Alberto Espay, a leading Parkinson’s specialist, says non-drug approaches should always come first. “We treat nausea like a symptom to be crushed with drugs,” he says. “But sometimes, the solution is simpler than we think.”
What to Do If You’ve Been Given the Wrong Drug
If you’ve received metoclopramide, prochlorperazine, or haloperidol and notice your tremors, stiffness, or freezing getting worse:- Stop the drug immediately. Don’t wait for your next appointment.
- Call your neurologist or Parkinson’s nurse. If you can’t reach them, go to the ER and say: “I have Parkinson’s. I was given a dopamine antagonist. I need help.”
- Bring your Medication to Avoid card. The American Parkinson Disease Association gives these out for free. They list every dangerous drug and are designed to be carried in your wallet.
- Document the reaction. Note the drug, dose, time, and symptoms. This helps your care team avoid it in the future.
Recovery can take days to weeks. Increasing your levodopa dose won’t fix it-because the problem isn’t low dopamine, it’s blocked receptors. The body needs time to clear the drug and reset.

How to Protect Yourself
You can’t control every doctor’s decision-but you can control your own safety.- Always tell every provider you see: “I have Parkinson’s. I cannot take dopamine-blocking antiemetics.” Say it again. Say it louder.
- Carry the APDA Medication to Avoid wallet card. Over 250,000 have been distributed since 2018. Patients with the card report a 40% drop in incorrect prescriptions.
- Ask your neurologist for a written list of safe and unsafe medications. Keep it in your phone and wallet.
- When admitted to hospital, give your medication list to the nurse and ask: “Is this antiemetic safe for Parkinson’s?”
- Use the Movement Disorder Society’s checklist: “Parkinson’s disease: verify antiemetic safety” should be written on every prescription.
Progress is happening. The Parkinson’s Foundation trained over 1,200 healthcare providers in 2023, cutting inappropriate prescriptions by 55% in participating hospitals. But until every ER doctor, dentist, and pharmacist knows the risk, you have to be your own advocate.
What’s Next? Better Options on the Horizon
Researchers are working on drugs that target nausea without touching the brain. The Michael J. Fox Foundation is funding a $1.2 million project to develop a new peripheral serotonin modulator-designed specifically for Parkinson’s patients. If successful, it could replace domperidone and ondansetron with something even safer.For now, the message is clear: Don’t let a simple case of nausea cost you your mobility. The right antiemetic exists. You just have to ask for it-and know what to say when they try to give you the wrong one.
Can I take metoclopramide if I have Parkinson’s disease?
No. Metoclopramide crosses the blood-brain barrier and blocks dopamine receptors, which can severely worsen Parkinson’s symptoms like tremors, rigidity, and freezing. It’s listed as a medication to avoid by the American Parkinson Disease Association and Parkinson’s UK. Even if you’ve taken it before without issues, the risk increases over time and with higher doses.
Is domperidone safe for Parkinson’s patients?
Yes, domperidone is the safest antiemetic for Parkinson’s patients because it doesn’t cross the blood-brain barrier. It works only in the gut to stop nausea. Studies show less than 2% risk of worsening motor symptoms. The main drawback is it’s not available as an injection in the U.S. and requires special FDA approval for oral use due to rare heart rhythm risks-though these are extremely low at standard doses.
What should I do if I’m given a dopamine antagonist by mistake?
Stop the medication immediately. Contact your neurologist or go to the emergency room. Tell them you have Parkinson’s and were given a dopamine-blocking antiemetic. Bring your Medication to Avoid card. Recovery can take days to weeks. Increasing your levodopa won’t fix it-the problem is receptor blockage, not low dopamine.
Are there natural ways to manage nausea with Parkinson’s?
Yes. Ginger (1 gram daily), eating small frequent meals, staying hydrated, and sitting upright after eating can significantly reduce nausea. Timing your levodopa at least 30 minutes before meals also helps. These methods are often more effective and safer than drugs. Dr. Alberto Espay recommends trying them before reaching for medication.
Why do doctors keep prescribing metoclopramide to Parkinson’s patients?
Because it’s cheap, widely available, and many doctors-especially in emergency rooms-aren’t trained in Parkinson’s-specific drug interactions. A 2022 study found only 37% of ER physicians knew metoclopramide was dangerous for Parkinson’s patients. It’s a systemic education gap, not a medical oversight. Patient advocacy and awareness cards are helping reduce this, but vigilance is still essential.
Every year, thousands of Parkinson’s patients are hospitalized because of a simple medication error. You don’t have to be one of them. Know your drugs. Know your risks. Speak up.

Post A Comment