Pharmacy Systems: How Medications Are Managed, Safety Checked, and Delivered in Canada
When you pick up a prescription, you’re not just getting a pill—you’re relying on a complex web of pharmacy systems, the structured processes and technologies that ensure drugs are made, tracked, dispensed, and monitored safely. Also known as drug distribution networks, these systems connect manufacturers, pharmacists, regulators, and patients in real time to prevent mistakes and protect health. It’s not magic. It’s barcode scans, lot number tracking, automated alerts, and strict rules that stop the wrong drug from reaching your hands.
Behind every safe medication is a sterile manufacturing, the controlled environment where injectables and IV drugs are made without contamination. Also known as aseptic processing, this step is non-negotiable—a single speck of dust can turn a lifesaving drug into a deadly one. These systems follow GMP compliance, the global standards that force manufacturers to prove every batch meets quality rules. Also known as current Good Manufacturing Practices, they’re why your insulin or chemotherapy doesn’t come with a warning label about mold. And once it leaves the lab, the drug enters another layer: drug safety monitoring, the global watch system that tracks side effects after a drug hits the market. Also known as pharmacovigilance, this network, including tools like VigiBase, collects reports from doctors and patients worldwide to catch hidden risks—like a new interaction between statins and antifungals that could wreck your muscles. These systems don’t just react—they predict. When the FDA flags a manufacturing flaw in 2025, it’s because these systems caught a pattern before patients got hurt.
And then there’s the human side: how generic drug distribution, the flow of low-cost copies of brand-name drugs through pharmacies and insurers. Also known as generic medication supply chains, this system saves billions—but also creates confusion. Look-alike, sound-alike names, mixed-up packaging, and PBM reimbursement rules can turn a simple refill into a mistake. That’s why modern pharmacy systems now include double-check software, color-coded labels, and electronic alerts that flag potential errors before they happen. Whether it’s adjusting a blood thinner dose for obesity, tracking a recalled implant, or making sure your EpiPen works when you need it, these systems are the invisible safety net keeping you alive.
What you’ll find below are real stories from inside these systems—the failures, the fixes, and the quiet tech that keeps your meds safe. No fluff. Just what matters when your health is on the line.
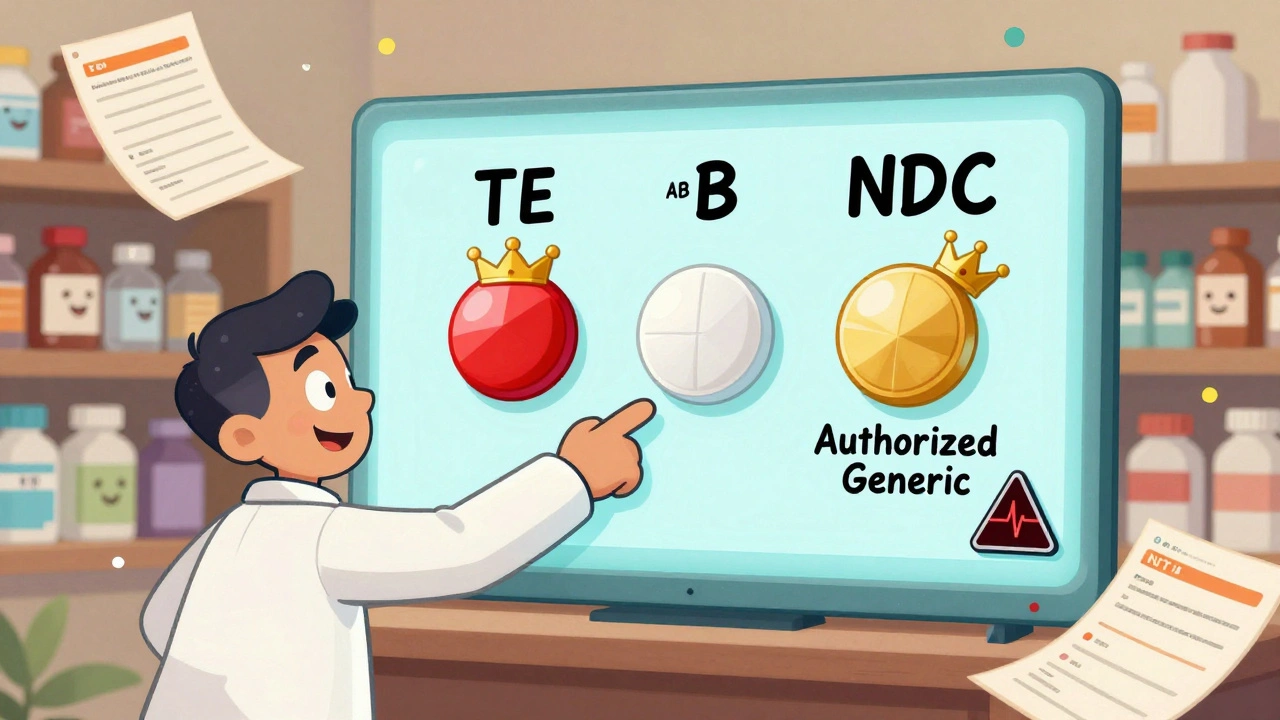
Generic vs Brand Identification in Pharmacy Systems: Best Practices for Accurate Medication Management
Learn how pharmacy systems accurately identify generic and brand-name drugs using NDC codes, TE ratings, and FDA guidelines. Best practices for safety, cost savings, and patient trust.
Read More