Brand Drugs: What They Are, How They Differ from Generics, and What You Need to Know
When you hear brand drugs, the original, patent-protected versions of medications developed by pharmaceutical companies. Also known as originator drugs, they’re the first to hit the market after years of research and clinical trials. These aren’t just names on a bottle—they’re the foundation of modern medicine. But after the patent expires, generics enter the scene, identical in active ingredients but often costing a fraction of the price. So why do brand drugs still exist? And should you care which one you take?
The difference isn’t in how they work—it’s in how they’re made and sold. pharmaceutical manufacturing, the complex process of producing drugs under strict quality controls for brand drugs involves proprietary formulas, exact packaging, and heavy marketing. That’s why a brand-name pill might cost $10 while the generic version is $2. But here’s the catch: the FDA requires generics to match brand drugs in strength, dosage, and how they’re absorbed by your body. So if your doctor says the generic is fine, it usually is. Still, some patients report differences in side effects or effectiveness. Why? It could be inactive ingredients—dyes, fillers, or coatings—that vary between brands and generics. These don’t treat your condition, but they can affect how the pill feels or dissolves.
drug pricing, the system that determines how much you pay for medication is messy. Brand drugs carry high prices to recoup R&D costs, but once generics flood the market, prices drop—sometimes dramatically. Yet, in some cases, even with multiple generics, prices stay high due to market consolidation or supply chain issues. And when a brand drug is the only option—like with biologics or complex injectables—you’re stuck with the cost. That’s why understanding your options matters. Some insurance plans push generics, others cover brand drugs with lower copays. Knowing your plan’s rules can save you hundreds a year.
Then there’s medication safety, how well a drug works without causing harm. Brand drugs have years of real-world data behind them. Generics, while tested, don’t always have the same long-term tracking. That’s why some patients—especially those on narrow therapeutic index drugs like warfarin or thyroid meds—stick with the brand. It’s not about trust in the generic—it’s about consistency. If your body reacts to a specific filler or coating, switching brands can trigger side effects. Your pharmacist can help you track these changes.
What you’ll find below isn’t just a list of articles. It’s a practical guide to the real-world side of brand drugs: how they’re made, why they cost what they do, when generics might not be enough, and how to protect yourself from errors or unsafe practices. From manufacturing flaws flagged by the FDA to how drug interactions can turn a safe pill into a danger, these posts cut through the noise. You’ll learn how to spot red flags in your prescriptions, understand why some drugs don’t have generics yet, and make smarter choices without overpaying.
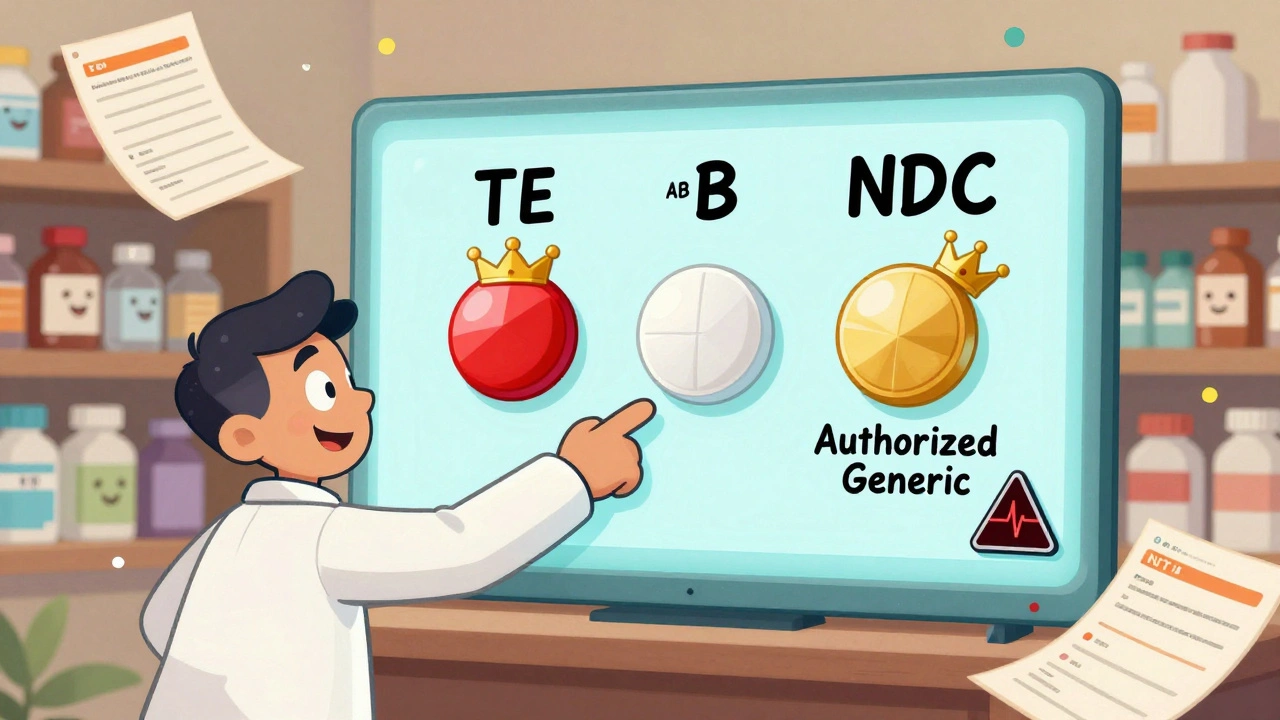
Generic vs Brand Identification in Pharmacy Systems: Best Practices for Accurate Medication Management
Learn how pharmacy systems accurately identify generic and brand-name drugs using NDC codes, TE ratings, and FDA guidelines. Best practices for safety, cost savings, and patient trust.
Read More