When a single psychiatric medication isn’t enough, doctors often turn to psychiatric medication combinations. This isn’t experimental-it’s standard practice for people with treatment-resistant depression, bipolar disorder, or severe anxiety. But here’s the catch: switching from brand-name drugs to generics in these combinations can be risky, and most patients don’t know it.
Why Combine Medications at All?
Many people start with one antidepressant-say, sertraline or escitalopram. But if symptoms don’t improve after 6 to 8 weeks, the next step isn’t always a new drug. Often, doctors add a second medication to boost the first. This is called augmentation. One of the most common combinations is an SSRI or SNRI with a low-dose atypical antipsychotic like aripiprazole. The FDA approved this combo in 2014 after trials showed it improved remission rates by nearly 24% compared to placebo. Another well-studied option is Symbyax, a fixed-dose pill combining fluoxetine and olanzapine. It’s designed specifically for people who haven’t responded to antidepressants alone. Other combinations include:- SSRI + buspirone for lingering anxiety without the risk of dependency
- bupropion + SSRI to fix sexual side effects caused by SSRIs
- lithium + anticonvulsants like valproate for bipolar disorder
Generic Substitution: The Hidden Risk
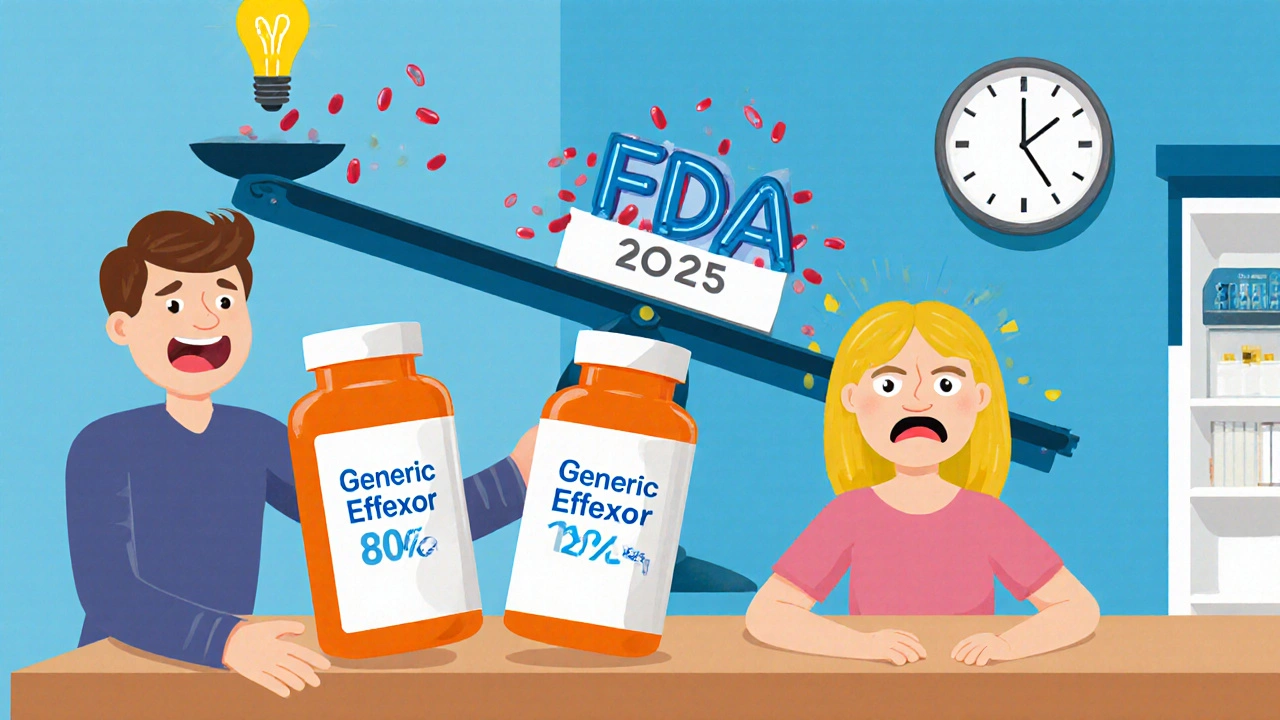
Generic drugs are cheaper. That’s why insurers push them. But in psychiatric care, cost savings can come at a steep price. The FDA says generics must be 80% to 125% as effective as the brand-name version. That’s a 45% window. For blood pressure or cholesterol meds, that’s usually fine. For psychiatric drugs, especially in combinations, it’s not. A 2019 study of nearly 28,500 patients found that switching from brand-name to generic SSRIs led to a 22.3% higher chance of treatment failure. That means more relapses, more hospital visits, more suffering. Why? Because small changes in how a drug is absorbed can throw off a carefully balanced system. Take venlafaxine ER (Effexor XR). It releases serotonin and norepinephrine in a precise 2:1 ratio. Generic versions use different bead technologies. One manufacturer’s version might release too much norepinephrine early on. Another might delay release too long. The result? Mood swings, panic attacks, or worse. The same problem hits lithium. Its therapeutic range is razor-thin: 0.6 to 1.2 mmol/L. A drop below 0.6 can trigger depression. A rise above 1.2 can cause tremors, confusion, or kidney damage. A 2018 case series from the University of British Columbia showed three bipolar patients went from stable to manic within two weeks of switching to a generic lithium formulation-even though the dose didn’t change. Their blood levels dropped from 0.85 to 0.55 mmol/L. And then there’s bupropion XL. In 2012, the FDA issued a warning after 137 reports of breakthrough depression and anxiety linked to certain generic versions. Patients reported sudden mood crashes, irritability, and even suicidal thoughts. The issue? Inconsistent drug release. Some generics release the full dose too fast. Others release it too slowly. Neither works like the original Wellbutrin XL.Real Stories, Real Consequences
Online forums are full of stories that mirror the research. On Reddit’s r/depression, a top thread from May 2023 titled “Generic switch ruined my carefully balanced med cocktail” has over 1,200 upvotes and nearly 300 comments. People write about:- Switching from brand Lamictal to Apotex generic-then Zoloft suddenly stopped working
- Switching Abilify generics and having obsessive thoughts return with full force
- Generic fluoxetine causing akathisia (a terrifying inner restlessness) that landed someone in the ER
How to Stay Safe If You’re on a Combination
You can’t avoid generics forever. But you can protect yourself. First: Know your meds. Write down every drug you take, including the manufacturer. If you’re on aripiprazole, is it from Mylan? Teva? Aurobindo? Keep that list. If you’re switched, ask: “Which generic is this?” Second: Don’t switch during a crisis. If you’re in a depressive episode or feeling unstable, don’t let your pharmacy switch your meds. Wait until you’re stable. That’s when your body can handle small changes. Third: Get tested. For lithium, valproate, carbamazepine, or clozapine-get a blood level check 7 to 14 days after any switch. Even if you feel fine. A level that looks “normal” on paper might be too low for you. Fourth: Track your symptoms. Use a simple journal. Rate your mood, sleep, energy, and anxiety on a scale of 1 to 10 every day for two weeks after a switch. If your score drops by 2 points or more, call your doctor. Don’t wait. Fifth: Ask for the same manufacturer. If you’ve been stable on a specific generic brand, ask your doctor to write “Dispense as written” or “Do not substitute” on your prescription. Many pharmacists will honor that.What’s Changing in 2025?
The system is starting to wake up. In May 2023, the FDA proposed tighter bioequivalence standards for extended-release psychiatric drugs-narrowing the range from 80-125% to 90-111%. That’s still not perfect, but it’s a step. The Department of Veterans Affairs now requires patients on stable combination therapy to stay on the same generic manufacturer for at least 12 months. Since that rule started, psychiatric hospitalizations dropped by nearly 19%. Authorized generics-brand-name drugs sold without the brand name-are becoming more common. Symbyax now has an authorized generic. That means the exact same pills, just cheaper. Ask your doctor if one exists for your meds. By 2025, the FDA plans to release product-specific bioequivalence guidelines for 27 high-risk psychiatric combinations. That’s huge. It means regulators will finally recognize that not all generics are created equal.
Who Should Avoid Generic Switches?
Not everyone needs to panic. But these groups should be extra cautious:- People on lithium, valproate, or carbamazepine (narrow therapeutic index)
- Those on more than two psychiatric medications
- Anyone who’s had a bad reaction to a generic before
- Patients with bipolar disorder or treatment-resistant depression
- People taking bupropion XL or venlafaxine ER
The Bottom Line
Generic drugs saved billions. That’s good. But when it comes to psychiatric combinations, one-size-fits-all doesn’t work. Your brain isn’t a machine that can be recalibrated with a new pill batch. It’s a delicate system built over months-or years-of careful dosing. If you’re on a combination, don’t assume generics are safe. Ask questions. Track your symptoms. Demand blood tests when needed. And if your doctor pushes a switch without explaining the risks, get a second opinion. The goal isn’t to avoid generics forever. It’s to make sure you’re the one in control-not the pharmacy, not the insurer, not the algorithm that picks your meds based on cost. Your mental health is worth more than a few dollars saved on a prescription.Can I safely switch from brand-name to generic psychiatric meds?
It depends. For single medications like fluoxetine or sertraline, most people switch without issue. But if you’re on two or more psychiatric drugs-especially lithium, valproate, bupropion XL, or venlafaxine ER-the risk of destabilization increases. Always consult your prescriber before switching, and never switch during an active episode.
Why do generics sometimes make psychiatric symptoms worse?
Generic drugs must be 80-125% as bioavailable as the brand name. That’s a huge range. For drugs with narrow therapeutic windows-like lithium or anticonvulsants-even a small drop in absorption can push you below the effective level. For extended-release meds like bupropion XL or venlafaxine ER, differences in bead technology can change how quickly the drug hits your bloodstream, leading to mood swings, anxiety, or relapse.
Which psychiatric generics are most likely to cause problems?
The most problematic generics include: bupropion XL (due to inconsistent release profiles), venlafaxine ER (because of altered serotonin/norepinephrine ratios), lithium carbonate (due to its narrow therapeutic range), and lamotrigine (where slight changes can trigger rashes or mood shifts). Studies show these have the highest rates of adverse outcomes after substitution.
Should I ask my doctor to write “Do Not Substitute” on my prescription?
Yes-if you’re on a combination therapy or have had a bad reaction to a generic before. Many states allow pharmacists to substitute unless the prescription says “Dispense as Written” or “Do Not Substitute.” This is legal and widely accepted. It doesn’t mean you can’t get generics-it just means you get the same one you’ve been stable on.
What should I do if I think my generic meds are making me worse?
Don’t stop taking your meds. Contact your prescriber immediately. Keep a symptom journal (mood, sleep, energy, anxiety) for at least two weeks. Ask for a blood level test if you’re on lithium, valproate, or carbamazepine. If your doctor dismisses your concerns, seek a second opinion from a psychopharmacologist. Your symptoms matter.
Are authorized generics safer than regular generics?
Yes. Authorized generics are made by the original brand-name manufacturer but sold without the brand name. They contain the exact same ingredients, fillers, and release mechanisms as the brand. For example, the authorized generic of Symbyax is identical to the branded version. If available, they’re the safest generic option for complex combinations.
Is there a way to test if a generic will work for me before switching?
Not directly-but you can reduce risk. Ask your doctor to check your blood levels before and 7-14 days after switching. Track your symptoms daily. If you’ve had a bad reaction to a generic before, avoid that manufacturer. Some pharmacies keep records of which generic you’ve taken successfully-ask them.


Post A Comment