Warfarin-NSAID Risk Calculator
Assess Your Bleeding Risk
Enter your warfarin dose and other risk factors to see how NSAIDs affect your bleeding risk.
Risk Assessment Results
Enter your information to see your risk level
Key Risk Factors
- Warfarin dose >40 mg/week: 2.5x higher risk
- Low INR (<1.5): 3.8x higher risk
- Gastrointestinal issues: 4.1x higher risk
- Taking multiple interacting medications: 2.9x higher risk
Safer Alternatives
If you need pain relief:
- Acetaminophen (up to 3,000 mg/day)
- Topical NSAIDs (gels/creams)
- Physical therapy
- Heat/cold therapy
Never take NSAIDs without consulting your doctor or anticoagulation clinic.
Imagine you’re on warfarin to prevent a stroke or blood clot. You’ve got your routine down: take your pill at the same time every day, get your INR checked regularly, avoid leafy greens that mess with vitamin K. Then you twist your knee. The pain is sharp. You reach for ibuprofen or naproxen - something over the counter, something quick. That’s when things get dangerous.
Warfarin and NSAIDs don’t just mix poorly. They create a perfect storm for bleeding. And it’s not some rare side effect. This interaction is well-documented, studied, and deadly serious. Every year, thousands of people on warfarin end up in the hospital because they took an NSAID without knowing the risk.
How Warfarin Works - And Why It’s Already a Balancing Act
Warfarin isn’t a simple blood thinner. It’s a vitamin K antagonist. That means it blocks your body’s ability to make key clotting factors: II, VII, IX, and X. These proteins need vitamin K to activate. Without them, your blood takes longer to clot - which is exactly what you want if you’re at risk for clots.
Your doctor monitors this with a number called INR - the International Normalized Ratio. A normal INR is around 1.0. For someone on warfarin, it’s usually kept between 2.0 and 3.0. Go above 4.0? Your bleeding risk spikes. Drop below 1.5? You’re not protected enough from clots.
Keeping INR stable is tricky. Diet, other meds, even antibiotics can throw it off. That’s why regular blood tests are non-negotiable. But adding an NSAID? That’s like slamming the brakes on your stability.
How NSAIDs Make Things Worse
NSAIDs - drugs like ibuprofen, naproxen, diclofenac, and even aspirin - work by blocking enzymes called COX-1 and COX-2. That reduces inflammation and pain. But here’s the catch: COX-1 is also needed to make thromboxane A2, a molecule that helps platelets stick together and form clots.
When you take an NSAID, platelets become sluggish. They can’t do their job properly. That’s why people on NSAIDs sometimes bleed longer from cuts. Now, combine that with warfarin, which already slows clotting from the inside. The result? A double hit on your body’s ability to stop bleeding.
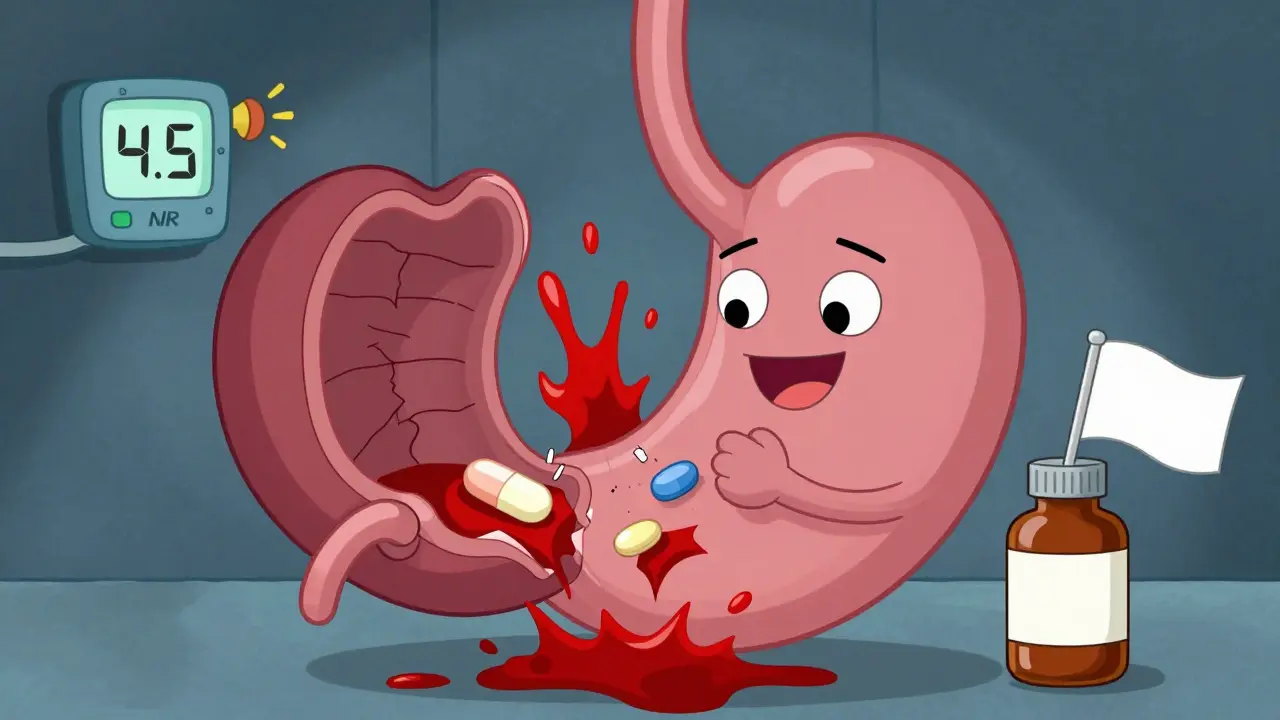
And it’s not just platelets. NSAIDs also damage the stomach lining. They reduce protective prostaglandins, leaving your gut more vulnerable to ulcers and bleeding. Warfarin doesn’t cause ulcers. But if you already have one, warfarin turns a slow leak into a hemorrhage.
The Numbers Don’t Lie - Bleeding Risk Skyrockets
Studies don’t just say “be careful.” They give hard numbers.
A 2019 analysis from the European Society of Cardiology found that people taking warfarin and an NSAID together had more than double the risk of bleeding compared to those on warfarin alone. That’s a 2.09 times higher chance of bleeding - anywhere.
But not all NSAIDs are equal. Some are far worse:
- Naproxen: 4.1 times higher bleeding risk
- Diclofenac: 3.3 times higher
- Ibuprofen: 1.79 times higher
Naproxen isn’t just common - it’s often recommended for arthritis. But for someone on warfarin? It’s one of the riskiest choices.
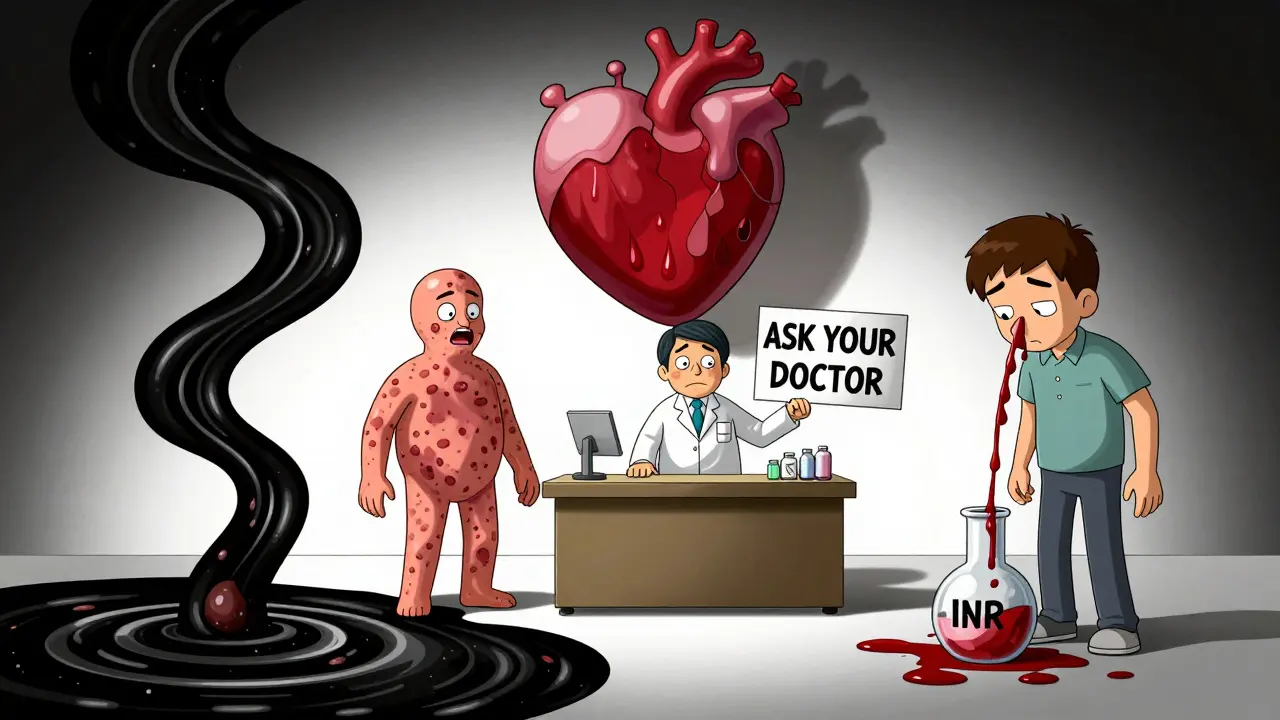
And where does the bleeding happen? The gut is ground zero. One study found a 2.24 times higher risk of gastrointestinal bleeding. Brain bleeds? 3.22 times more likely. Lung and urinary tract bleeds? Also significantly higher. Even anemia from slow, unnoticed bleeding spiked nearly threefold.
Who’s Most at Risk?
This isn’t a one-size-fits-all danger. Some people are sitting ducks.
- Those on high-dose warfarin (>40 mg per week)
- People with low baseline INR (meaning their blood clots more easily - so the drop from NSAIDs hits harder)
- Anyone taking other drugs that interact with warfarin - like antibiotics, antifungals, or even some herbal supplements
- Those already on proton pump inhibitors (PPIs) for stomach issues - a sign they’re already at risk
One study of 98 patients showed that 39.8% had their INR jump by 15% or more after starting an NSAID. That’s nearly 4 out of 10. And INR spikes don’t wait. They can happen within days.
What About Other Blood Thinners?
What if you’re on a newer drug like dabigatran or rivaroxaban? Are you safer?
Not really. While the mechanism is different - these drugs don’t touch vitamin K - they still carry bleeding risk. Studies show NSAIDs raise bleeding risk with DOACs too. One study found that among people on dabigatran, NSAID users had significantly more major bleeding events. GI bleeding made up 40% of those cases. Non-GI bleeding? 60%.
The bottom line? If you’re on any anticoagulant, NSAIDs aren’t a safe bet.
What Should You Do Instead?
Don’t panic. Pain doesn’t have to mean NSAIDs.
Acetaminophen (paracetamol) is the go-to alternative. Up to 3,000 mg per day is generally safe for people on warfarin. It doesn’t affect platelets or the stomach lining. It’s not as strong for inflammation, but for headaches, muscle aches, or joint pain? It works.
Other options:
- Topical NSAIDs - gels or patches applied to the skin. They don’t enter your bloodstream the same way, so risk is much lower.
- Physical therapy - for back or knee pain, movement often beats pills.
- Heat or cold packs - simple, free, and surprisingly effective.
- Low-dose capsaicin cream - helps with nerve-related pain.
If you absolutely must use an NSAID - say, for severe arthritis - talk to your doctor. They might:
- Prescribe the lowest dose for the shortest time
- Give you a proton pump inhibitor (like pantoprazole 40 mg daily) to protect your stomach
- Check your INR within 3 to 5 days of starting the NSAID
- Monitor you weekly while you’re on both
And never, ever start an NSAID without telling your anticoagulation clinic or pharmacist. Even if it’s just one pill.
Why This Still Happens - And Why It’s a Problem
Here’s the scary part: despite all the evidence, doctors still prescribe this combo. A 2022 study found that nearly 3 out of 10 warfarin users got an NSAID prescription within a year. That’s not a mistake. It’s a system failure.
Patients don’t always know. Pharmacists can’t catch every interaction. Primary care docs are rushed. And NSAIDs? They’re sold next to candy in the pharmacy aisle. People think, “It’s just ibuprofen.”
But it’s not. It’s a trigger for bleeding - and bleeding from warfarin and NSAIDs doesn’t always show up as a nosebleed or bruise. Sometimes it’s internal. Fatigue. Dizziness. Dark stools. Abdominal pain. Those are signs you’re losing blood slowly - and you might not notice until it’s too late.
What to Watch For - Bleeding Warning Signs
If you’re on warfarin and take an NSAID (even once), know these red flags:
- Bleeding that won’t stop - cuts, nosebleeds, gums
- Unusual bruising - large, unexplained patches
- Dark, tarry stools - a sign of GI bleeding
- Bright red blood in stool or urine
- Severe headache, dizziness, vision changes - possible brain bleed
- Unexplained fatigue or shortness of breath - could mean anemia from internal bleeding
If any of these happen, get medical help immediately. Don’t wait. Don’t assume it’s “just a side effect.”
And if you’re thinking about starting an NSAID? Talk to your doctor first. Ask: "Is this safe with my warfarin?" If they say yes, ask: "How often should my INR be checked?" If they can’t answer, find someone who can.
Can I take ibuprofen with warfarin if I only take it once in a while?
Even occasional use of ibuprofen with warfarin can spike your INR and raise bleeding risk. A single dose can trigger an INR increase in some people, especially if you’re on a higher warfarin dose or have other risk factors. It’s not worth the gamble. Use acetaminophen instead.
Is naproxen worse than ibuprofen with warfarin?
Yes. Naproxen carries a 4.1-fold higher bleeding risk compared to warfarin alone - the highest among common NSAIDs. Ibuprofen is still risky (1.79-fold), but naproxen is consistently linked to more severe outcomes. Avoid naproxen entirely if you’re on warfarin.
Why does meloxicam increase bleeding risk more than other NSAIDs?
Meloxicam has been identified in studies as an independent risk factor for INR elevation in warfarin users. It may interfere with how warfarin is metabolized in the liver, leading to higher drug levels in the blood. It’s not just about platelet effects - it’s a metabolic interaction too. Avoid meloxicam if you’re on warfarin.
Should I stop taking NSAIDs before a blood test?
Yes - if you’ve taken an NSAID in the past week, tell your provider. NSAIDs can affect INR for several days after the last dose. Your test might show a falsely high INR, leading to unnecessary warfarin dose changes. Always disclose NSAID use before your INR check.
Are topical NSAIDs safe with warfarin?
Topical NSAIDs (gels, creams, patches) are generally safer because very little enters the bloodstream. For localized pain - like a sore knee or shoulder - they’re a good alternative. But avoid large areas or long-term use. Always check with your doctor first.


Post A Comment