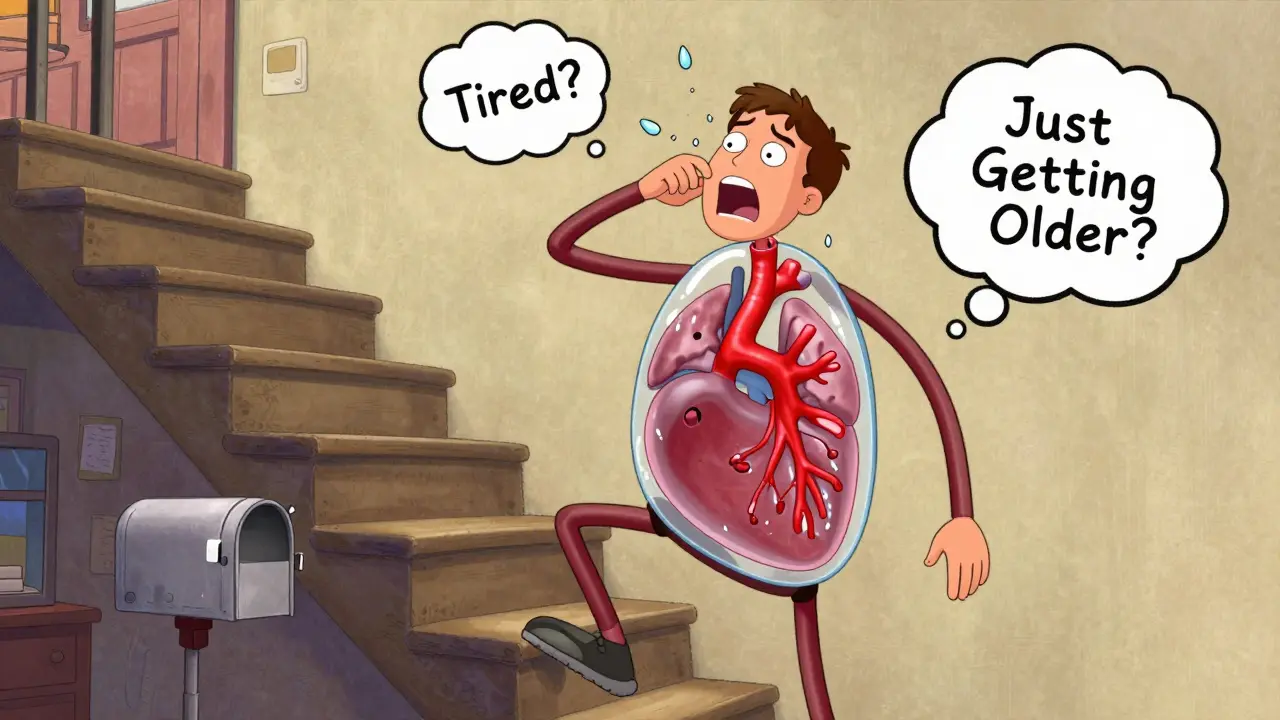
When you start getting out of breath climbing stairs, or feel like you can’t catch your breath after walking to the mailbox, it’s easy to blame it on age, being out of shape, or even allergies. But if that breathlessness keeps getting worse-especially if it’s paired with swelling in your ankles, chest pain, or dizziness-you could be dealing with something far more serious: pulmonary hypertension.
What Exactly Is Pulmonary Hypertension?
Pulmonary hypertension (PH) isn’t just high blood pressure in your lungs. It’s a progressive condition where the arteries carrying blood from your heart to your lungs become narrowed, stiff, or blocked. This forces your right ventricle-the chamber that pumps blood to your lungs-to work harder and harder. Over time, that strain can weaken the muscle, leading to right heart failure. It’s not rare: about 1 in 100 people worldwide have it, and women are twice as likely to be diagnosed as men.
The World Health Organization groups PH into five types, but the most common and most dangerous is Group 1: pulmonary arterial hypertension (PAH). This is where the problem starts in the lung arteries themselves. Other groups are tied to heart failure (Group 2), lung diseases like COPD (Group 3), blood clots in the lungs (Group 4), or unknown causes (Group 5). Each type needs a different approach to treatment.
Early Symptoms Are Subtle-But They Add Up
Most people with PH don’t wake up one day with a chest pain or collapse. Instead, symptoms creep in slowly. You might notice:
- Shortness of breath during normal activities-like walking to the kitchen or folding laundry
- Feeling unusually tired, even after a full night’s sleep
- Swelling in your ankles, legs, or belly
- Chest pressure or pain, especially when you’re active
- Dizziness or fainting spells, particularly when standing up or exerting yourself
- A bluish tint to your lips or skin (cyanosis)
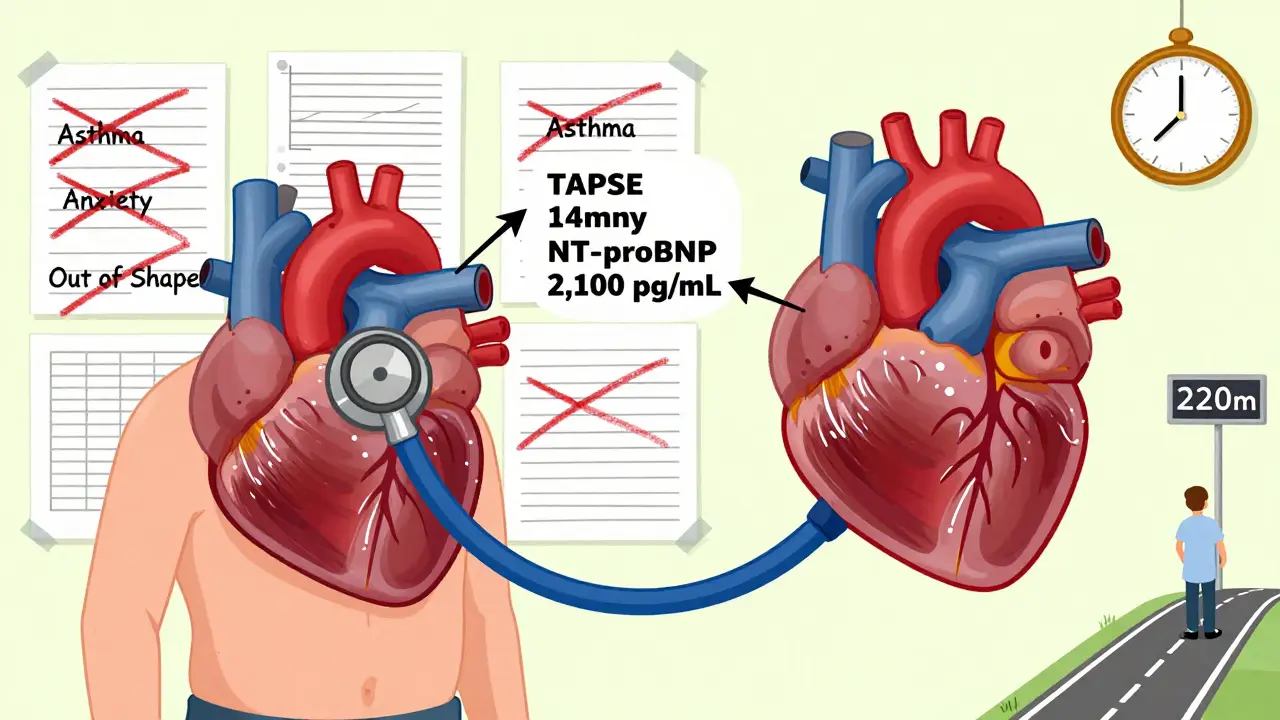
These signs are often mistaken for asthma, anxiety, or just getting older. In fact, studies show that nearly 80% of PH patients were misdiagnosed at first. One patient on a support forum said, “My doctor told me I was just out of shape for 18 months while my 6-minute walk distance dropped from 500 meters to 220.” That delay in diagnosis is dangerous. Every month without treatment lets the right side of your heart deteriorate further.
Right Heart Strain: The Silent Consequence
When the pulmonary arteries get stiff, the right ventricle has to pump harder to push blood through. That extra workload causes measurable changes:
- Right ventricular hypertrophy: The muscle wall thickens beyond 5mm (seen on echocardiogram)
- Right ventricular dilation: The chamber stretches out, growing larger than 22 cm²
- Reduced TAPSE: A measurement called tricuspid annular plane systolic excursion drops below 17mm, showing the heart can’t contract properly
These aren’t just numbers on a screen-they’re warning signs. A TAPSE under 17mm means your heart is struggling. A 6-minute walk test distance under 380 meters doubles your risk of death within a year. And if your BNP or NT-proBNP blood levels rise above 180 pg/mL or 1,400 pg/mL respectively, that’s a clear signal your heart is under severe stress.
Doctors don’t just rely on one test. They look at the whole picture: how you feel, what your blood tests show, what your echo reveals, and how far you can walk. That’s why a specialist won’t make a diagnosis based on symptoms alone.
Diagnosis: Why Right Heart Catheterization Is Still the Gold Standard
Many patients think an echocardiogram is enough. And while it’s a great first step, it’s not perfect. Studies show it’s only 56% specific for PH-it often overestimates pressure by 10 to 15 mmHg. That means people get told they have PH when they don’t… or worse, they’re told they’re fine when they actually do.
The only way to know for sure is right heart catheterization. This procedure measures the actual pressure in your pulmonary arteries. The current diagnostic cutoff? A mean pulmonary arterial pressure greater than 20 mmHg at rest. That’s a change from the old standard of 25 mmHg, which means more people are being diagnosed earlier.
Yes, it’s invasive. There’s a small risk of complications-like arrhythmia or bleeding-but the benefits far outweigh the risks. As Dr. Nazzareno Galiè says, “Non-invasive methods cannot replace direct pressure measurement.” Without catheterization, you can’t tell if the problem is in your lungs (Group 1 or 3) or if it’s caused by a weak left heart (Group 2). That distinction changes everything about your treatment.
Modern Therapy: From Single Drugs to Combination Treatments
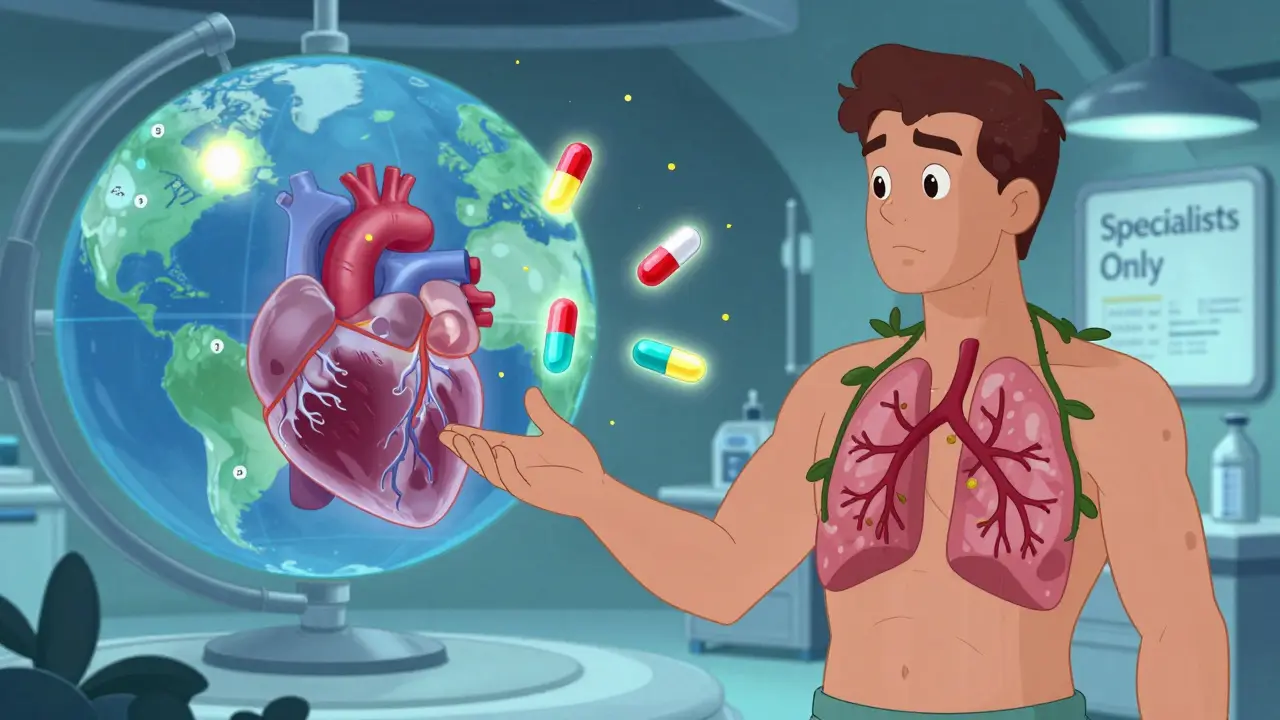
Twenty years ago, PH meant a life expectancy of less than three years. Today, thanks to targeted therapies, 5-year survival has jumped to over 60%. That’s not magic-it’s science.
There are now 14 FDA-approved drugs for PH, grouped into five classes:
- Endothelin receptor antagonists (like bosentan, macitentan)
- PDE-5 inhibitors (sildenafil, tadalafil)
- Prostacyclin analogs (epoprostenol, treprostinil-given by IV, inhaled, or under the skin)
- Soluble guanylate cyclase stimulators (riociguat)
- Novel agents like sotatercept, approved in 2021, which targets the TGF-β pathway to actually reverse artery thickening
Back in 2010, most patients started on one drug. Now, 68% of patients begin with two or three together. Why? Because PH attacks the body through multiple pathways. Hitting just one target isn’t enough. Combination therapy has become the new standard for moderate to severe cases.
For the most advanced cases, continuous IV prostacyclin therapy is used. That means a central line and a portable pump that runs 24/7. It’s not easy, but for many, it’s the difference between being bedbound and walking again.
What’s on the Horizon?
The future of PH treatment is exciting. Sotatercept isn’t the end-it’s the beginning. The LIBERTY trial is testing let-7 microRNA as a biomarker to detect right heart strain before symptoms even appear. Researchers are also testing drugs like dichloroacetate to improve how the right ventricle uses energy, which could help it recover.
But the biggest challenge isn’t the science-it’s access. Only 35 specialized PH centers exist in the U.S., and many patients wait over 30 days for insurance approval to get the drugs they need. Minority patients face delays nearly 50% longer than white patients. That gap isn’t just unfair-it’s deadly.
How to Get the Right Care
If you suspect PH, don’t wait. Go to a specialist. Look for a center certified by the Pulmonary Hypertension Care Center program. These clinics have teams: cardiologists, pulmonologists, pharmacists, nurses, and social workers-all trained in PH. They don’t just treat your numbers-they treat you.
Ask for:
- A right heart catheterization if your echo suggests PH
- Regular TAPSE and NT-proBNP monitoring
- A 6-minute walk test every 3 to 6 months
- A discussion about combination therapy if you’re in WHO Functional Class II or higher
And if your doctor dismisses your symptoms as “just anxiety” or “you’re getting old”-get a second opinion. PH doesn’t care about your age or your fitness level. It only cares if you’re diagnosed early enough to treat it.
Can pulmonary hypertension be cured?
There is no cure for pulmonary hypertension yet, but modern treatments can significantly slow its progression and improve quality of life. Some patients, especially those with chronic thromboembolic PH (Group 4), may be eligible for a surgical procedure called pulmonary thromboendarterectomy, which can remove blood clots and restore normal pressure. For others, combination drug therapy and close monitoring can stabilize the condition for many years.
Is pulmonary hypertension the same as regular high blood pressure?
No. Regular high blood pressure (systemic hypertension) affects arteries throughout your body and is measured in your arm. Pulmonary hypertension only affects the arteries going from your heart to your lungs. The pressures are different, the causes are different, and the treatments are completely separate. You can have one without the other.
How do I know if my treatment is working?
Your doctor will track several markers: your 6-minute walk distance, your NT-proBNP blood levels, your right ventricular function on echo (especially TAPSE), and your WHO functional class. If your walk distance increases, your BNP drops, and your heart’s pumping improves, your treatment is working. If you’re still getting winded climbing stairs or your swelling returns, it’s time to adjust your therapy.
Can I exercise with pulmonary hypertension?
Yes-under supervision. Inactivity makes your heart weaker. Many PH patients benefit from carefully monitored pulmonary rehabilitation programs that include light aerobic exercise, strength training, and breathing techniques. Avoid heavy lifting or holding your breath. Always check with your PH specialist before starting any new routine.
Why do I need to see a specialist instead of my regular doctor?
Pulmonary hypertension is rare and complex. Most general practitioners see fewer than one case in their entire career. Specialists know how to interpret catheterization results, recognize subtle echo changes, manage complex drug combinations, and spot early signs of right heart failure. They also have access to clinical trials and advanced therapies not available elsewhere. Seeing a PH center is not optional-it’s essential for survival.

Post A Comment