Diabetic gastroparesis isn’t just a nuisance-it can wreck your blood sugar control, make you feel full after one bite, and turn meals into a chore. When your stomach won’t empty properly because of nerve damage from diabetes, standard treatments like metoclopramide often come with serious side effects. That’s where domperidone comes in. It’s not approved in the U.S., but in Canada, Europe, and Australia, doctors have been using it for years to help people with this condition. So, does it actually work? And is it safe?
What Is Diabetic Gastroparesis?
Diabetic gastroparesis happens when high blood sugar damages the vagus nerve, which controls how fast food moves from your stomach to your small intestine. Without that signal, your stomach sits there, slowly digesting food-or not digesting it at all. Symptoms include nausea, vomiting undigested food, bloating, early fullness, and unpredictable blood sugar spikes. It’s not rare: up to 50% of people with type 1 diabetes and 30% of those with type 2 develop it over time. The real problem? It makes diabetes harder to manage. If food doesn’t move on schedule, insulin timing becomes guesswork.
Why Domperidone Is Different
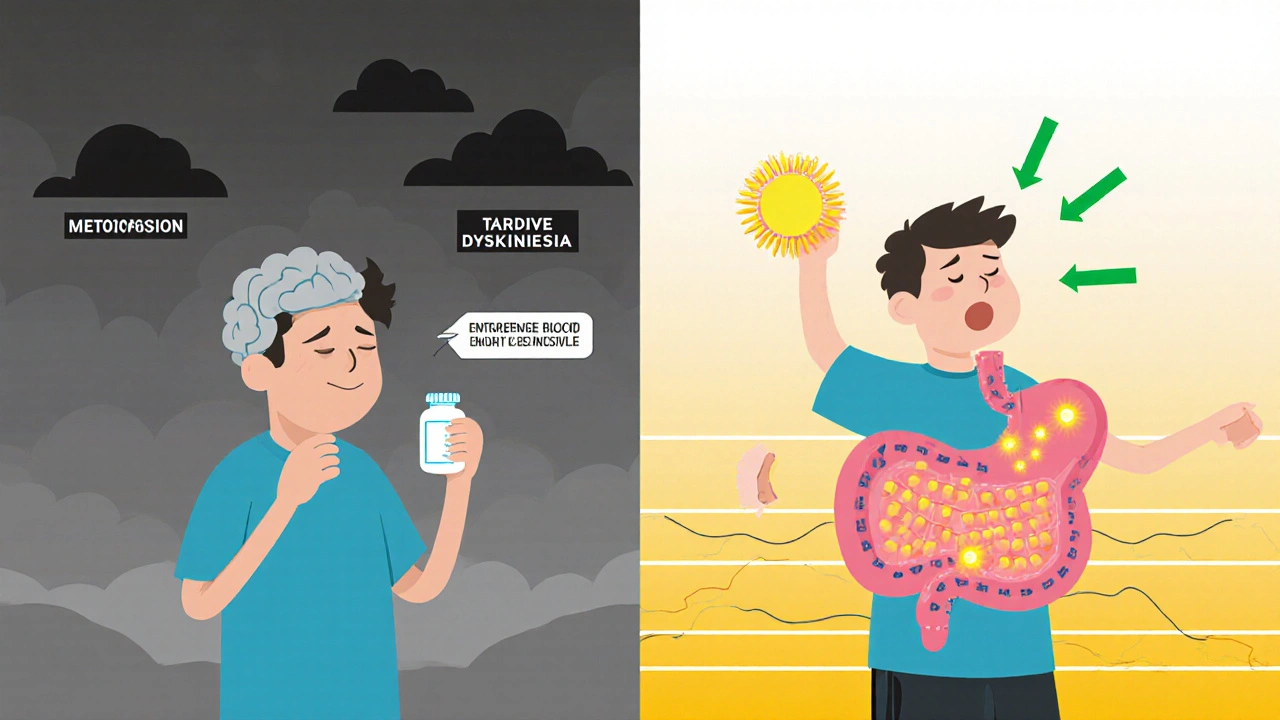
Most drugs for gastroparesis work by stimulating stomach contractions. Metoclopramide, the go-to in the U.S., does that-but it can cause depression, fatigue, and even a rare movement disorder called tardive dyskinesia after long-term use. Domperidone, on the other hand, doesn’t cross the blood-brain barrier. That means it acts only on the stomach and intestines, not the brain. It blocks dopamine receptors in the gut, which boosts contractions and speeds up gastric emptying. No brain exposure = fewer neurological side effects. That’s why many doctors outside the U.S. see it as a safer alternative.
How Effective Is Domperidone?
Several clinical studies show clear benefits. A 2021 randomized trial published in Diabetes Care followed 120 patients with diabetic gastroparesis for 12 weeks. Half took domperidone 10 mg three times daily before meals; half took a placebo. Those on domperidone had a 40% improvement in gastric emptying time, measured by a standard breath test. They also reported 50% less nausea and vomiting. Another study from the UK in 2023 tracked 85 patients over six months. Nearly 70% said their quality of life improved significantly-better sleep, fewer emergency visits, and more stable blood sugar levels.
It’s not a cure. Domperidone doesn’t repair nerve damage. But it helps the stomach work better with what’s left. For many, it’s the first treatment that actually reduces vomiting without making them feel drugged or dizzy.
Why Isn’t It Available in the U.S.?
The FDA hasn’t approved domperidone for gastroparesis, and it’s not sold legally in the U.S. The concern? A small risk of heart rhythm problems, specifically a prolonged QT interval, which can lead to dangerous arrhythmias. That risk is real-but it’s mostly tied to high doses (over 30 mg per day), pre-existing heart conditions, or mixing it with other drugs that affect heart rhythm. In countries where it’s approved, doctors screen patients first: no history of heart disease, no electrolyte imbalances, no other QT-prolonging meds. Doses are kept low-10 mg three times a day, max. With proper monitoring, the risk is very low.
Some U.S. patients get domperidone through compounding pharmacies or international pharmacies, but that’s not regulated. If you’re considering this route, work with a doctor who understands how to monitor for side effects.
Who Should Consider It?
Domperidone isn’t for everyone. It’s best for people who:
- Have confirmed diabetic gastroparesis via gastric emptying scan
- Can’t tolerate metoclopramide due to side effects
- Are otherwise healthy with no heart rhythm issues
- Have tried diet changes and blood sugar control without success
It’s not recommended if you have:
- History of cardiac arrhythmias or QT prolongation
- Severe liver disease
- Are taking antifungals, certain antibiotics, or antidepressants that affect heart rhythm
Before starting, your doctor should order an ECG to check your QT interval. Repeat it after 2-4 weeks on the drug. Blood tests for potassium and magnesium are also important-low levels increase heart risks.
What to Expect When Taking It
Most people start feeling better within a week. Nausea eases first. Appetite returns. Vomiting becomes less frequent. It’s not magic-you still need to eat small, low-fat, low-fiber meals. Avoid carbonated drinks. Stay upright for two hours after eating. But unlike metoclopramide, you won’t feel like you’re floating or numb. Many patients report feeling more like themselves again.
Side effects are usually mild: dry mouth, headache, or mild abdominal cramps. Serious ones-like irregular heartbeat-are rare when used correctly. If you feel your heart racing, get an ECG right away.
Alternatives and Complementary Approaches
Domperidone isn’t the only option. Other drugs like erythromycin (an antibiotic that also stimulates stomach contractions) can help short-term, but tolerance builds fast. Gastric electrical stimulation is an option for severe cases, but it’s expensive and invasive. Botox injections into the stomach pylorus have shown mixed results.
Lifestyle matters just as much. Eating five tiny meals a day, avoiding high-fat foods, and chewing food thoroughly can improve symptoms on their own. Some patients benefit from gastric pacing devices or even experimental therapies like stem cell injections, but those are still in trials.
Domperidone works best when paired with tight blood sugar control. If your HbA1c is above 8%, no drug will fix your gastroparesis fully. Fix the glucose first. Then add domperidone as a tool to help your stomach keep up.
Final Thoughts
If you’re living with diabetic gastroparesis and standard treatments haven’t worked, domperidone deserves a serious look. It’s not perfect. It’s not FDA-approved. But for thousands of people outside the U.S., it’s made life bearable again. With proper screening, low dosing, and regular heart monitoring, the benefits far outweigh the risks for most patients. Talk to your doctor-not to get a prescription, but to understand if you’re a candidate. And if your doctor says no because it’s not approved here, ask if they’re willing to help you explore safe, monitored access. Your stomach shouldn’t be the reason your diabetes stays out of control.
Is domperidone approved for gastroparesis in the U.S.?
No, domperidone is not FDA-approved for any use in the United States. It’s available only through compounding pharmacies or international sources, and its use is considered off-label. Doctors may help patients access it under special circumstances with proper monitoring.
How long does it take for domperidone to work for gastroparesis?
Most patients notice reduced nausea and improved appetite within 3 to 7 days. Full improvement in gastric emptying and symptom control usually takes 2 to 4 weeks. It’s not an instant fix, but it works faster than many other treatments.
Can domperidone cause heart problems?
Yes, but only in rare cases when used incorrectly. The risk comes from high doses (over 30 mg/day), pre-existing heart conditions, low potassium or magnesium levels, or combining it with other drugs that prolong the QT interval. With proper screening and a standard dose of 10 mg three times daily, the risk is very low-lower than the risk of uncontrolled gastroparesis.
What’s the difference between domperidone and metoclopramide?
Both improve stomach emptying, but metoclopramide crosses the blood-brain barrier and can cause depression, fatigue, and movement disorders. Domperidone doesn’t enter the brain, so it avoids those side effects. Domperidone is generally safer for long-term use, but metoclopramide is the only FDA-approved option in the U.S.
Do I need to change my diet if I take domperidone?
Yes. Domperidone helps your stomach empty, but it doesn’t fix poor digestion. You still need to eat small, low-fat, low-fiber meals, chew thoroughly, and avoid carbonated drinks. Diet changes are essential-medication alone won’t solve everything.
Can I take domperidone with my diabetes medications?
Yes, but you’ll need to adjust your insulin timing. Since domperidone speeds up stomach emptying, food hits your bloodstream faster. That means your rapid-acting insulin may need to be taken closer to mealtime instead of 15-20 minutes before. Work with your endocrinologist to fine-tune your regimen.


Post A Comment